Medicine is much like politics. Both fields have an affinity to condense complicated multifaceted issues into value-laden phrases that add no actual value. These phrases permeate every discipline in medicine, and, as seen in politics, can change the way people view issues (ie. incentivizing doctors to have advance care planning discussions with patients being transformed into a simple phrase – death panels). Below are just several examples of value-laden yet valueless phrases in medicine and the reasons we use them:
- Failure to Thrive: an expression of linguistic laziness in which the provider is too busy to express the underlying issues such as depression, weight loss, or mobility issues. In adult medicine, it is only used in describing a constellation of symptoms in the very old in the hopes that no further investigation is needed, often with stunningly great success in its implementation. Antonym: acromegaly.
- Withdrawal of Care: an expression of extreme self-doubt as a healer in which the provider of care conveys a feeling that only treatments that are focused on cure can truly be considered care. The effect: family members feel abandoned if they choose anything but invasive life prolonging interventions. Antonym: “Full Treatment”.
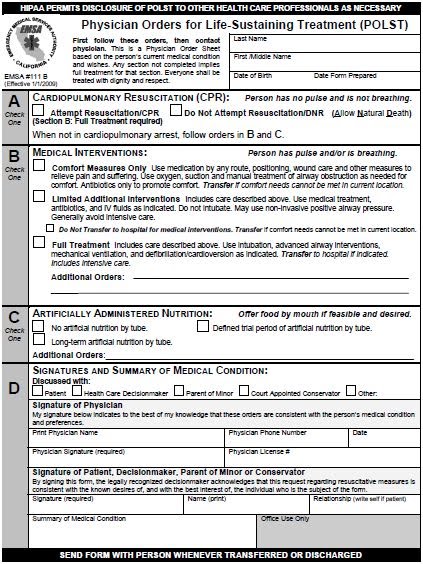
- Full Treatment: a phrase communicates that anything less than intubation, defibrillation, a-lines, peg tubes, and rectal tubes would constitute less than full treatment. A phrase that assumes that aggressive symptom management in home hospice from an interdisciplinary team of nurses, social workers, case managers, chaplains, and volunteers would be less rather than more treatment than in a hospital setting. A phrase that is fragment of a concept – waiting desperately for someone to add its relation to a goal (full treatment to ensure that he/she is without pain or suffering? Full treatment to ensure that he/she makes it to the birth of his granddaughter?). Antonym: Comfort care (which I won’t define as I’m not sure exactly what it is). Usage: see POLST section B
Why do we medical types love these words? Why do I hear the words “withdrawal of care” all the time in the ICU? Why is “Full Treatment” part of the POLST form – the very form that I hailed as the best thing since sliced bread in a previous post (I still think that way about the POLST despite this rant)? A classic children’s book, Fish is Fish by Leo Lionni , gives us a clue. Here is a summary (warning – spoiler alert):
Two friends, a minnow and a tadpole, are inseparable until the tadpole grows into a frog and leaves the pond to explore the world on land. When the frog returns to tell his friend of the extraordinary things he’s seen, the minnow, now a fish, imagines the animals that the frog is describing. The fish, though, can only comprehend these animals as taking a fish-like form (a bird is imagined to be a fish with wings). The lesson – people construct new beliefs/knowledge/skills based on their current beliefs/knowledge/skills.
“Withdrawal of care” and “full treatment” are both relatively new concepts with good intentions, however they are derived from traditional models of what “treatment” and “care” means. The traditional models are still the basis for most of our beliefs and govern most of what we do in medicine, including how health care providers are reimbursed. If a physician can bill handsomely for it, than, as you can pretty much guess, it probably would be included as “care” or as a “treatment”. If not, like a social work or chaplaincy visit, than it probably wasn’t important anyway and shouldn’t be considered “care”.
The truth for patients though is much different than the reality that our health care system attempts to create. Fully treating patients requires that we attend to the physical, social, psychological, and spiritual needs of both the patients and their loved ones. This care is more likely to occur in programs like hospice or PACE that have wandered away the stagnant pond of the traditional health care model.
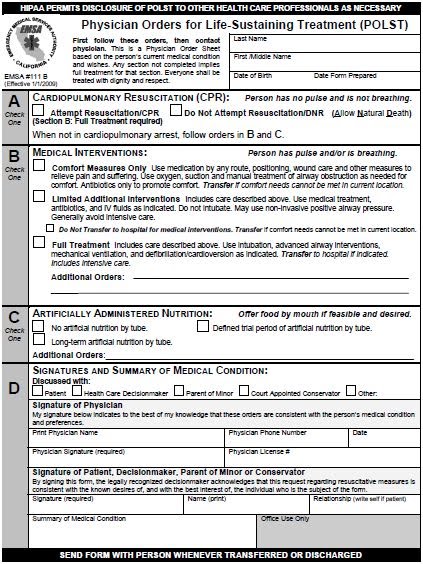
So how can we avoid value-laden phrases that add no value? Fort a start, it would be helpful if we stopped adding them to important end-of-life documents. This wouldn’t be so hard. For instance – here is section B of the POLST form with and without a pithy phrase (see picture for full POLST form):
[] Full Treatment: Includes care described above. Use intubation, advanced airway interventions, mechanical ventilation, and cardioversion as indicated. Transfer to hospital if indicated. Includes intensive care.
[] Include all care described above. In addition, use intubation, advanced airway interventions, mechanical ventilation, and cardioversion as indicated. Transfer to hospital if indicated. Includes intensive care.
Now which one of these two options did you think tells you more about someone’s treatment preferences? If you answered “they are both the same” than the addition of the phrase “Full Treatment” is at best a waste of ink. If you thought the addition of “Full Treatment” gave you a better idea of what a person would want then we have a much bigger problem than our domestic ink supply.
by: Eric Widera



