Attention all Geriatric, Palliative Medicine, and Primary Care Providers:
Act now to prevent the adoption of strict, punitive
regulations impacting opioid prescribing.
The proposed Center for Medicare and Medicaid Services (CMS) regulations
will significantly hamper our ability to provide individualized care for
patients with serious or life-limiting illnesses. Porter Storey, Executive Vice
President for the American Academy of Hospice and Palliative Medicine (AAHPM),
recently highlighted this urgent need at a University of Colorado Palliative
Medicine Grand Rounds, and AAHPM is currently drafting a letter of comment for
CMS. We thought it important enough to share with the Geripal community because
your stories matter. Time is of the essence.
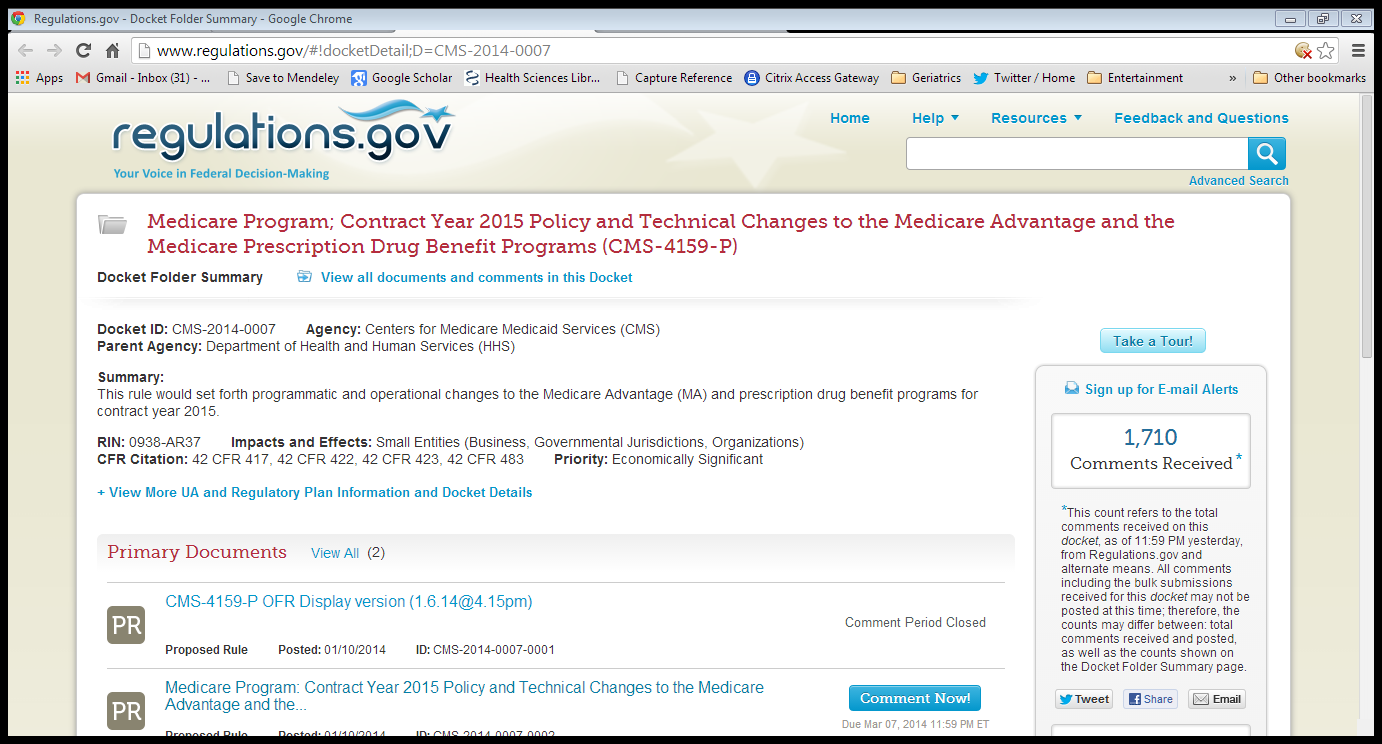
This is a call to action to comment onCMS-4159-P. The proposed rule revises
theMedicare Advantage program (Part C)
regulations and prescription drug benefit program (Part D) regulations. As stated in the Executive
Summary, one of the goals is to “strengthen
our ability to identify strong applicants for Part C and Part D program participation
and remove consistently poor performers.” While part of the intent of the
revision is to identify inappropriate prescribing of opioid and other
potentially harmful medications, thesenew guidelines may have significant unintended
consequences, including limiting access to appropriate symptom management for
patients with serious illnesses.
The proposed rule will 1) require a certification for
Medicare Part D prescribing abilities, and 2) could result in suspension or
revocation of all Medicare Part D privileges. The fine print is worrisome. The
last 2 pages of the 678 page document describe prescribing practices that could
result in revocation of Provider enrollment in the Medicare Part D program.
Specifically,
424.535 (14) Improper prescribing practices.CMS determines that the physician or eligible professional has
a pattern or practice of prescribing Part D drugs that falls into one of the
following categories:
- “Instance
where necessary evaluation could not have occurred” - “Prescribed
controlled substances in excessive doses, linked to overdoses” - “Prescribing
drugs for indications not medically accepted” - “Malpractice
suit where physician paid settlement to plaintiff”
Here are a few scenarios to show why you should be
worried:
1) A rural
primary care physician serving as medical director for the region’s only hospice
misinterprets the new rule and decides she can’t prescribe for patients she
hasn’t seen because they live 100 miles away and can’t come to the office. This
results in an entire region without access to appropriate palliative care.
2) A coroner draws opioid levels on a decedent with
cancer who was on stable, but high-dose opioids and mislabels the case an
opioid-related death resulting in loss of prescribing capabilities for a
palliative care doctor.
3) A pulmonologist raises concerns that a patient
was inappropriately prescribed opioids for dyspnea because the pulmonologist is
worried that opioids might raise the patient’s CO2 levels, causing harm. This results
in a claim that the opioid indications are not medically accepted, despite
increasing evidence of benefit.
AND, most importantly of all, you should be
concerned because the proposed regulations lack a description of any form of
due process by which providers would be able to describe the validity of their
prescribing practice.
In summary, the proposed rule, CMS-4159-P, has the
potential to severely limit the ability of providers who care for patients with
serious or life-limiting illnesses to provide patient-centered care. This aspect
of the regulation needs to be withdrawn or significantly revised to recognize
that so-called “improper prescribing practices” is a
nebulous concept without a solid scientific definition.There are examples of non-FDA approved uses of medications that
are considered best practice or standard of care in certain medical
specialties. As currently written, the regulations fail to describe how
improper prescribing practices will be identified and adjudicated. For
primary care physicians, who currently fill much of the need for symptom
management in advanced illnesses, the vague terms in this regulation jeopardize
their long-term ability to prescribe medications for any Medicare beneficiary
enrolled in the Part D program.
So, dear reader, please contact CMS. Tell a story of
a patient you care for, and how your goals are patient-centered care. Describe
how your patient wouldn’t be eligible for a clinical trial and thus, you are
using your medical judgment as you prescribe medications and make dose
adjustments based on treatment responses, like pain relief, quality of life, and
improved function. Describe how you do a significant amount of follow up and
care coordination with caregivers and your clinic team because your patient is
too ill to travel to your office. Describe your efforts to monitor for misuse
or abuse, and how you prescribe the lowest effective doses, which still may be
much higher than average doses that work for other patients outside of
palliative care.
Take
Action Now – Comments are due by March 7, 2014.
Please
submit electronic comments on this proposed rule to CMS. They read these comments!
They note, “A single, well-supported comment may carry more weight than a
thousand form letters.”
You
can read the PDF of the proposed rule here, but for time’s sake skip to the last 2
pages.
Then
you can submit your comments by following this link to Medicare
Program: Contract Year 2015 Policy and Technical Changes to the Medicare
Advantage and the Medicare Prescription Drug Benefit Programs
Suggestions for preparing your comments:
Consider commenting specifically on PART
424–CONDITIONS FOR MEDICARE PAYMENT, Section 424.535 – Revocation of
enrollment in the Medicare program. (pg 675-6)
- Describe
how this regulation will impact your patients - Be
concise but support your claims - Base your
justification on sound reasoning, scientific evidence, and/or how you will be
impacted - Address
trade-offs and opposing views in your comment - There is
no minimum or maximum length for an effective comment
By: Hillary Lum and Paul Tatum. Special thanks to Porter
Storey for raising our awareness, and members of the AAHPM policy committee for
quick review.
If you’ve read this far, take a few more minutes and
submit a comment to CMS. March 7 will be here soon!