by: Laura Petrillo (@lpetrillz)
There is increasing interest around the country in documenting patient preferences for life sustaining treatment, with the hope that patients may receive care in line with their goals and values during an emergency. Many states in the US do this through Physician Order for Life Sustaining Treatment (POLST) programs, which are active or developing in all but five states [1]. California has had a law in place since 2008 that mandates honoring a POLST, and on October 1st, 2014, the state will roll out a new version, the first revision since 2011. The changes are subtle, but there are definite shifts in language and emphasis that reflect larger themes.
Here we’ll take a look at how the new California version compares to POLST equivalents already in use in other states, and what the changes suggest about how attitudes about this important topic are shifting in our community.
What is a POLST?
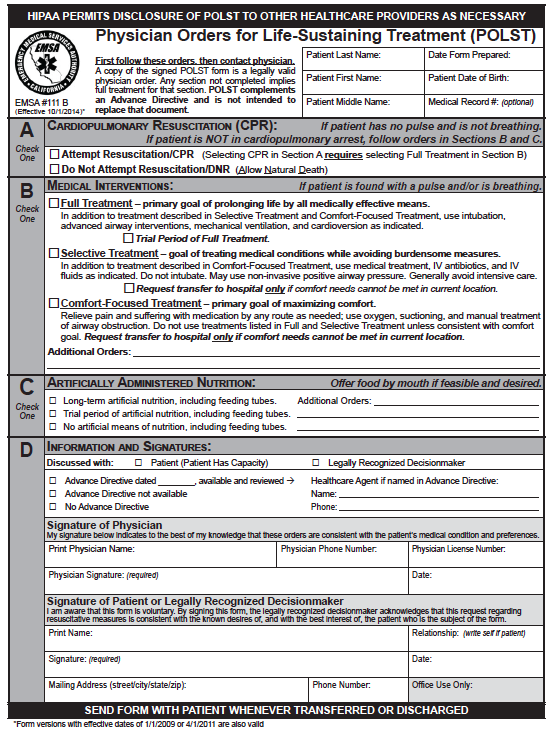
The POLST is an out of hospital physician’s order that indicates patient preferences for resuscitation and scope of treatment, intended to be completed for seriously ill or frail patients and to be followed by emergency medical providers. The choices for scope of treatment range from full treatment to comfort-focused measures, and in California, patients can also list their preferences for artificial nutrition. To be valid, the form needs to be signed by a physician and the patient, or the patient’s legally recognized decision maker.
Why fill out a POLST?
The goal of the POLST is to align the care that is provided in an emergency with what would be acceptable to a patient, to make sure that a patient’s wishes are honored even when he can’t speak for himself. Recent data from Oregon show that patients who filled out a POLST and chose “Comfort Measures Only” were less likely to die in the hospital (6.4%), compared to 34.2% of patients who did not have a POLST form, and 44.2% of patients who completed a POLST and chose “Full Treatment” [2].
What’s new in this version and how is it compare to other states?
The most important changes are:
1) The order of options in the first two sections has changed. Previously, Section A gave options “Attempt Resuscitation/CPR,” followed by “Do Not Attempt Resuscitation/DNR (Allow Natural Death).” In Section B, the first choice was the least aggressive, “Comfort Measures Only,” followed by “Limited Additional Interventions” and “Full Treatment.” Now, to be more consistent, Sections A and B both proceed from most aggressive to least aggressive.
Does order matter? As previously discussed on GeriPal, when the “default” choice on an advance directive presented to seriously ill patients was comfort care, with the option to strike this out and choose full code instead, 80% of patients stuck with the default choice, compared to 61% who chose comfort care on a standard advance directive [3]. Though that was a much more deliberate suggestion of a default than simply having a particular option listed first, one can imagine that order might subtly influence decision making, and reinforce our cultural bias that full treatment/full code is the default for all patients.
Of note, the Colorado POLST equivalent lists DNR first in Section A and “Comfort Measures” first in Section B, presenting the least aggressive options first. Oregon, Minnesota and New York’s POLST equivalents are discordant like California’s was before the change, with “Full Code” first in Section A and “Comfort Care” first in Section B. My favorite example of subtle bias in presentation of options is in Idaho’s POLST, where the full treatment option is called “Aggressive Interventions.”
2) The scope of treatment choices in Section B were renamed: “Limited Additional Interventions” was changed to “Selective Treatment” and “Comfort Measures Only” was changed to “Comfort-Focused Treatment.”
The changes are positive, and make less aggressive options feel more like a shift of focus, rather than that things are being taken away or withheld. Contrast this to New York’s POLST equivalent, the MOLST, in which full treatment option is “No limitations on medical treatments: the patient will receive all needed treatments.”
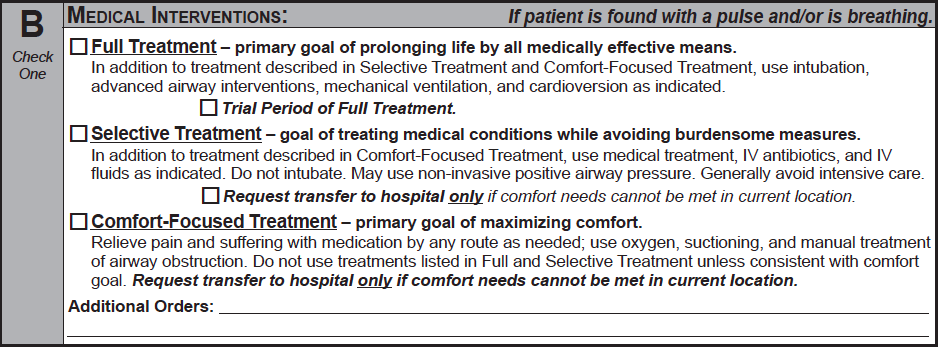
3) In Section B, goal statements have been added after each of the options to expand on the aims of each option and serve as a springboard for discussion. For example, the goal of “Selective Treatment” is “Treating medical conditions while avoiding burdensome measures.”
This is an improvement over the previous version, where the descriptions of Section B options focused solely on the type of additional interventions (antibiotics, fluids, intubation) that each option allowed beyond the least aggressive option listed above it.
While the idea of including goals certainly exciting, it is not unprecedented in the POLST world. The Oregon POLST provides similarly succinct overviews of each treatment plan that are similar to California’s goal statements. But the mother of all goal-oriented POLSTs is New Jersey’s, which just has a blank space in section A, titled “Goals of care.” The form provides the suggestion that providers ask patients, “What are your hopes for the future? Examples include but not restricted to: Longevity, cure, remission or Better quality of life….”
The easy criticism of New Jersey’s approach is that patients are unlikely to know in advance what their goals would be in an emergency, and would likely have different goals depending on the situation. It is impossible to imagine every scenario (“Well, I’d want to be cardioverted if it were unstable atrial fibrillation with rapid rate, but if a piano dropped on my head from the sky, I’d want quality over quantity”). But bravo, NJ, for thinking broadly—everyone is glad to get more of a vision of the patient on the page rather than her feelings about a la carte feeding tubes.
4) The last major change is that section B gives the option of checking a box for a “Trial Period” under the full treatment option.
Another exciting development. The concept of time-limited trials is nicely laid out by Timothy Quill in this JAMA article: “an agreement between clinicians and a patient/family to use certain medical therapies over a defined period to see if the patient improves or deteriorates according to agreed-on clinical outcomes” [4]. It may seem obvious that it’s a good idea to check in periodically to see if the plan of care is achieving the patient and medical team’s goals, but it happens surprisingly infrequently in practice. Though checking the box provides very nonspecific direction to future providers, including the suggestion of time limited trials in POLSTs to remind providers to reevaluate after starting a course of action is a terrific idea.
And that’s a wrap! At first glance, the changes are relatively minor, but one can sense a tectonic shift beneath, with an overall move toward a focus on goals and reevaluation of whether treatments are aligned with goals, rather than such a specific treatment-focused menu.
What do you think of the new POLST? Do you think it reflects how you talk about life-sustaining treatment with patients now, and if not, what could make it better? Do you think it will have any effect on how you have these conversations in the future? If you have experience with the other states’ versions of POLST, we’d like to hear about that too!
References
1. National POLST website. Available at: http://www.polst.org/programs-in-your-state/.
2. Fromme EK, Zive D, Schmidt TA, Cook JNB, Tolle SW. Association Between Physician Orders for Life-Sustaining Treatment for Scope of Treatment and In-Hospital Death in Oregon. J. Am. Geriatr. Soc. 2014;62(7):1246-1251.
3. Halpern SD, Loewenstein G, Volpp KG, et al. Default Options In Advance Directives Influence How Patients Set Goals For End-Of-Life Care. Heal. Aff. 2013;32 (2 ):408-417.
4. Quist TE, Holloway R. Time-limited trials near the end of life. JAMA 2011;306(13):1483-1484. Available at: http://dx.doi.org/10.1001/jama.2011.1413.



