
Does this sound like
you, or someone you know?
An 86-year-old female patient came in with her daughter. She
had Chronic Obstructive Pulmonary Disease (COPD), depression, anxiety, and was
brought in by her daughter because she has had trouble sleeping, mostly with
falling asleep, and less so with staying asleep. She had tried mirtazapine and
trazodone (other sleep medications) without success. Her daughter asked, “Can mom try melatonin?” and I
wondered: Is melatonin more effective than placebo as a treatment of insomnia?
I searched the terms “insomnia melatonin” on PubMed Clinical
Queries looking specifically for systematic reviews, which usually provide an
exhaustive summary of current literature and offer higher quality evidence than
individual journal articles. I found a review article summarizing results from
19 randomized-controlled trials with a total sample of 1683 participants. The
review looked at 3 outcomes: sleep latency (the amount of time it takes to fall
asleep), total sleep time, and sleep quality. For each of the outcome, it explored 3 of its components – objective
(actual amount of time), subjective (patients’ feeling of how long it takes),
and overall (both subjective and objective combined). Individual patient data
was used for analysis, and there was no publication bias on Egger’s test on any
of the outcome measures.
The results were consistent across the 19 studies included
in the review, and shown below in a table format. Of note, for sleep quality,
the review reported the findings as standardized mean difference, because each
study used different scales to measure sleep quality. This makes it difficult
to interpret what the findings mean to patients.
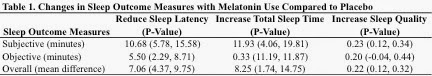
In summary, it seems that melatonin helps patients feel that
they fall asleep faster, sleep longer, and get better quality sleep, although
in reality the actual effects are not as great as what patients feel. Also,
although statistically significant, these improvements may not be clinically
significant for every patient. For example, falling asleep faster by 7.06
minutes might not mean much for many patients, especially when we compare these
effects to those of other sleep medications, such as non-benzodiazepine sleep
aides (reduce sleep latency by 12.8 to 17 minutes), or benzodiazepine sleep
aides (reduce sleep latency by 10.0 to 19.6 minutes).
Back to the patient: Although
I was not impressed with melatonin’s ability to reduce sleep latency by 7
minutes, melatonin is safe, cheap, with no side effects of addiction, so we
decided to give it a try. At a follow-up visit, patient reported no benefits
from melatonin, and the search for a better sleep aide continued.
Take-home points:
1. Melatonin is safe, cheap, with no side effects of
addiction.
2. Melatonin makes patients believe they have better sleep,
although when measured in reality, the improvements are small.
– By June Howell, a geriatrics fellow who blogs at https://medium.com/@junehowellmd
and tweets @junehowellmd
This post is part of the #GeriCases
series, in which we discuss a clinical case in geriatrics and the
attempt to provide patient-centered care with the use of best available
evidence.
Ravishankar Ramaswamy, MD
@RavRamaswamy
Section Editor, #GeriCases
Reference: Ferracioli-Oda E1, Qawasmi A, Bloch MH
Meta-analysis: melatonin for the treatment of primary sleep disorders. PLoS
One. 2013 May 17;8(5):e63773. doi: 10.1371/journal.pone.0063773.
Image source: Moyan Brenn, no modification



