While it has taken years to popularize the word “palliative” (I have to confess that the word still does not roll nicely off my accented tongue), it is remarkable how the recent negative press related to the issues addressed in the Newsweek article on rethinking end of life care have managed to gain significant traction swiftly. I worry that all this sensationalism will distract from real and important discourse on sensitive topics like exploring the underlying suffering beneath patients’ requests for hastening death. On a related note, Dr. Susan Block from Harvard Medical School has authored a very timely video module entitled : Patient Requests to Manage Life’s Final Chapter: Assessment and Palliation.The module is hosted on a Stanford curricular LMS, please note that you have to register and sign up to get access to it (takes 2 business days) . On a positive note, the module is free full text and has a interactive video case study intertwined into the module, pre and post test video questions.
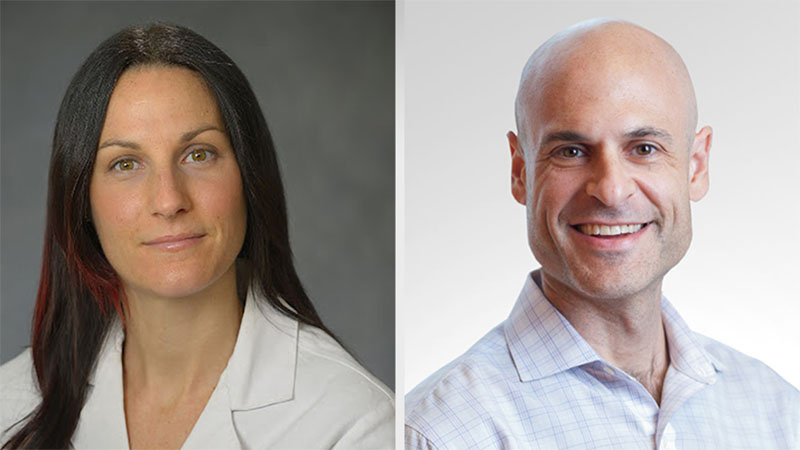
Case study: The clip above is about Emily, a 56 year old dancer with advanced ovarian cancer s/p multiple rounds of chemo with minimal response. After struggling with multiple distressing symptoms due to the cancer and the treatments for almost three years, Emily decides to stop chemotherapy. Her oncologist, Dr. Stevenson (played by the extremely talented oncologist, Dr. Beth Martin, from Stanford), wants to start Emily on a promising experimental chemotherapy agent. However, Emily just stops coming to her Oncology appointments and instead writes a letter to Dr. Stevenson asking for help with hastening her end. Dr. Stevenson, who totally did not see this coming, is taken aback and reaches out to her colleague and palliative care expert, Dr. Susan Block. Check out the video clip above to see a conversation between Dr. Stevenson and Dr. Block (played by the extremely talented Dr. Susan Block from Harvard).
Case study credits: Case written, directed and produced by VJ Periyakoil, MD. All characters ( except Dr. Block’s character) appearing in this case study are fictitious. Any resemblance to real persons, living or dead, is purely coincidental.