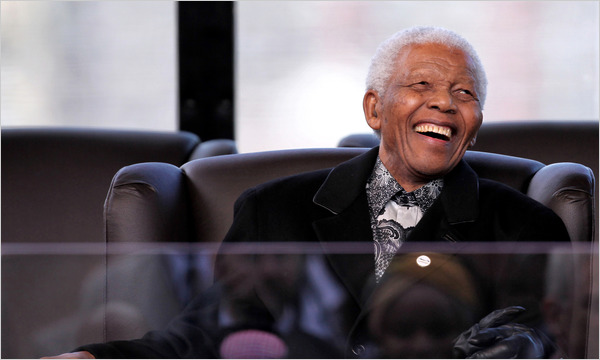
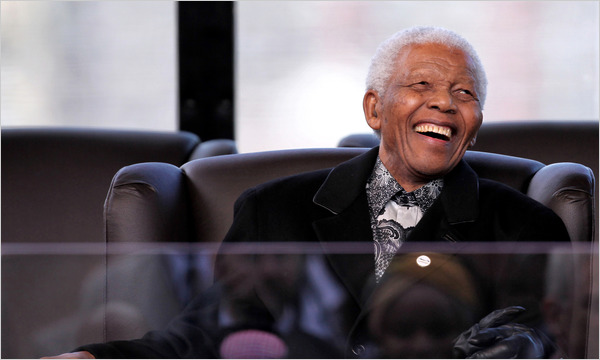
There is a wonderful article in the New York Times, written by Celia Dugger, that discusses the aging of Nelson Mandela. I found something really appealing about this article. It discusses the frailties Mr. Mandela is facing, frailties that are common in 91 year olds. Yet rather than portraying the disabilities of aging in a negative light, the article seems to convey a certain reverence for aging—The while hair, frail body, trouble walking, hearing impairment, and short term memory problems only add to Mandela’s iconic status.
I found the public reverence for the aging Mandela, grounded in his epic struggle and courage, to be analogous to the more personal reverence we and our patients’ families feel for parents and grandparents as they age—reverence that is not diminished, but enhanced, when they develop these frailties.
I wonder if Geriatricians need to do more as a discipline to convey this reverence. Much of the science of Geriatrics is focused on preventing and delaying these fraities, and this is as it should be. But I sometimes wonder if we talk too much about so-called, “successful aging,” holding up as the ideal the 91 year tennis player doing their daily jog. No doubt this is a wonderful thing, as rare as it is. But perhaps the better ideal for our discipline is the 91 year old with trouble walking, lots of medical problems, and in need of caregiver assistance, yet revered by their family and living a great quality of life.



