No man, not even a doctor, ever gives any other definition of what a nurse should be than this — ‘devoted and obedient.’ This definition would do just as well for a porter. It might even do for a horse. It would not do for a policeman.
-Florence Nightingale, 1859
This is Nurses’ Week (May 6-12) and the celebration of Florence Nightingale’s birthday. Please take a moment to celebrate the nurses in your life. Florence Nightingale was the first to publicly decry the sorry reputation of nurses – as in the quote – but nurses remain vastly underappreciated for the work they do. Let’s take a moment to consider how nurses contribute to the interdisciplinary teams in the nursing home, the hospital, the hospice, and the clinic.
I think we’ve underappreciated the role of nurses as teachers. I must give thanks first to the nurses who have taught me and continue to teach me. As a physician-in-training and now as a junior attending, nurses have taught me at least as much about clinical medicine and caring for patients as any other group except patients. From nurses I’ve been amazed to learn what home health and hospice can accomplish at home, the limits of what can be done in the nursing home, and really practical advice like patients should lie on their left side when infusing an enema (it’s a straighter shot into the colon, if you were wondering).
Nurse practitioners were the first ones to practice gerontology and palliative care in many places, and have been the senior-most clinical mentors to many of us. When I was at the Brigham, when we ran out of ideas for treatment of complex pain, we often turned to Maureen Lynch, the NP and senior clinician on the palliative care team for advice. Patrice Villars is the senior clinician at the SF VAMC and I routinely look to her for advice on how to approach complex and challenging patients. Nurse practitioners, being both clinicians and nurses, are uniquely able to navigate challenging issues and dynamics that arise between nurses, physicians, patients, and families.
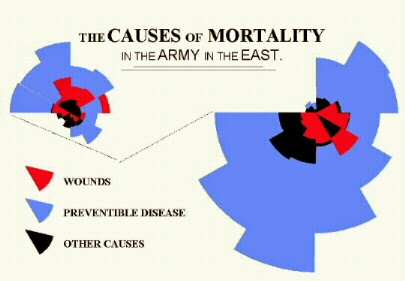
There is an expression, “Nurses are on the front lines,” that certainly applied in Florence Nightingale’s time – she described being “up to her elbows in blood,” caring for British soldiers in the Crimean war – and still applies today. Nurses are there, in the room, when the patient and family have stopped putting on their best face for the doctors. They have contributed to countless family meetings, as witnesses to the everyday experiences of patients and families: joy and suffering, hope and fear, loss and renewal.
And physicians, let’s stop claiming ownership of the nurses we work with, as in, “This is my nurse X.” It’s demeaning and emphasizes a hierarchy that is antithetical to highly functioning interdisciplinary teams. Thanks, Patrice, for this perspective – you see, I’m learning!
So say thank you to each other if you’re a nurse, and if not, say thank you to the nurses you know! Happy Nurses Week!