Every time I get off the phone with Christian Sinclair (AAHPM board member, Pallimed rock-star, and social media guru) I become very excited about the wonderful community of bloggers we have online. So in today’s post I just want to highlight four outstanding posts that have popped up online in the last week.
1. This week’s best post on grammar: Care Coordination Is Not a Noun
Chris Langston from the health AGEnda (the John A. Hartford Foundation blog) argues that far to often “we act as if care coordination was a thing that might come in a box, brought to us by a care coordinator.” This post is well worth reading for the examples used to describe his conclusion, which is elequently stated as “care coordination is a system property that requires careful redesign of plans and procedures, new hardware and new software, and yes, new people in new positions, but none of these features taken alone defines care coordination.”
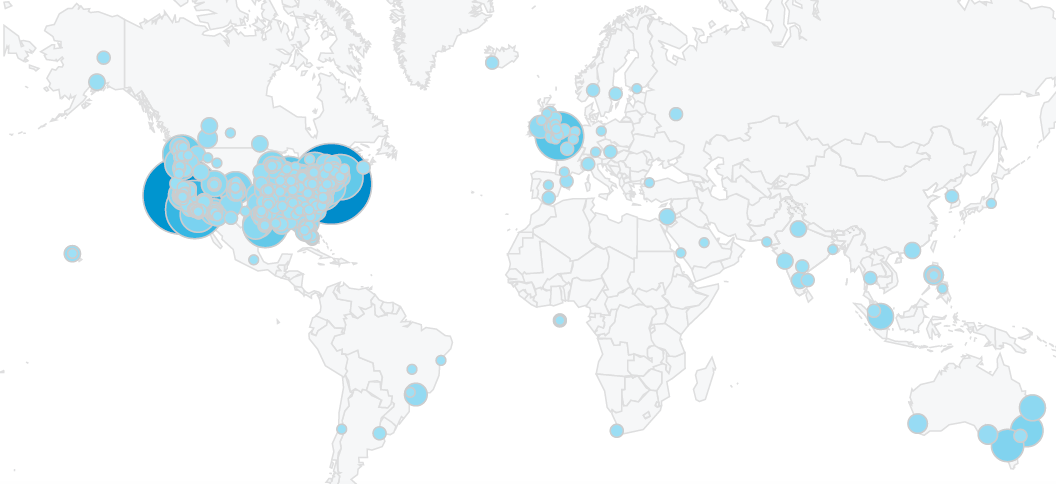
2. This week’s best post on the intersection between geriatrics and palliative care – Cartography of EOL Pain
Brian McMichael from Pallimed reviews an article that GeriPal’s very own Alex Smith was the lead author on – “The epidemiology of pain during the last 2 years of life”. Brian breaks down the article in the first half of his post and comes away with some take away points that I feel highlight the need for more geriatric content within palliative care:
“I have felt like arthritis is this incidental given, dwarfed by the likes of angina, dyspnea, acute fracture, and malignant pain, etc.; a kind of tell-me-something-I-don’t-already-know entity. It’s surprising to see this common, benign condition produce such a large overall, and then burgeoning burden of pain at end-of-life.”
3. This week’s best post on Community – Palliative Care Grand Rounds
Compassion & Choices is hosting this month’s Palliative Care Grand Rounds. If you are not sure what grand rounds is check it out for a flavor of some online offerings.
4. This weeks best post on why we need to be online – Why Doctors Should Care About Social Media
Bryan Vartabedian from 33 Charts lists 6 reasons why doctors (I’ll expand this to all health care professionals) should be using social media. The most salient reason for both geriatrics and palliative care is the last – the world needs to see us as part of the global dialog. He ends (as do I) with the following:
“If each of us shared even small, regular contributions (doctor-doctor, doctor-patient, doctor-policy maker) the impact would be dramatic.”
by: Eric Widera