Over the last two weeks I have had four different second year residents from several institutions ask me about when they should start thinking about applying for fellowships. Some of these residents were applying for palliative care positions, and some geriatrics positions. The answer I gave them unfortunately was the same:
“If you are interested in a 2013 spot at UCSF, start getting your application together for an interview season that will likely start in the fall and end in the early winter.”
The overwhelming response that I got was “really? I just finished internship.” Although, I’m pretty sure a more verbose response was going on inside their head akin to “are you &#!@% kidding me!”
There was one response though that really caught me off guard and made me worry about what the lack of a match meant for the future of our fields. The resident replied to my statement by saying:
“but our residency director told us that we now don’t even have to worry about the applying for fellowships until the beginning of third year.”
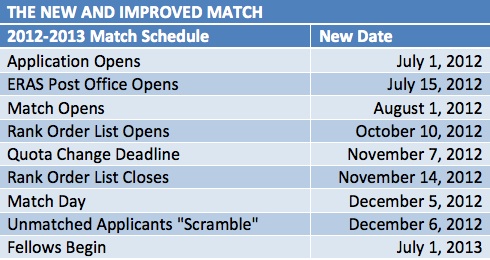
This response is now very true, except of course for two fellowship programs – geriatrics and palliative care. As we discussed in a previous post about the match, all the other subspecialties in internal medicine have agreed that residents deserve the opportunity to gain more exposure to future career options prior to deciding upon a particular fellowship path. These other subspecialties (by these I do mean all other subspecialties) are delaying ‘match day’ and have therefore moved decisions regarding which program residents would like to end up at until well into third year.
Both geriatrics and palliative care though are stuck with a dysfunctional matchless system that shows blatant disregard for learners. This is not just my opinion. Thanks to the wonders of social media, we are starting to see more stories about what being ‘matchless’ means to the future of our fields. In his Pallimed post, Brian McMichael tells an all too common story about his experiences in applying for a fellowship. Here is a brief excerpt:
“The diversity among programs in their respective timelines for application review, interviewing, and how and when to do what about making offers is frankly stunning. My process was cut short by a spoils-to-the-swift ethic. Because of the asynchronous timelines, I had to decline interview offers from programs I was very interested in. Given the inherent power disparity in the roles and the dynamics involved, I did not believe I had the latitude to walk away from offers from great programs in order to “explore my options” further. Perhaps my issue, but I doubt mine alone.”
I encourage you to read all of Brian’s post. I’d also love to hear from fellows or faculty on what there concers are with a match for our fellowship programs. Or, if you are a fellow (or faculty) and would like to share your experience, please comment at either Pallimed or GeriPal with your own story (or email me directly).
by: Eric Widera



