There is an estimated 6.7 million emergency hospitalizations every year in the US. One out of every 67 of these hospitalizations is due to an adverse drug event.
This is just one of the many interesting, although somewhat questionable points made by Daniel S. Budnitz and colleagues NEJM article titled “Emergency Hospitalizations for Adverse Drug Events in Older Americans”. It’s a compelling article that, in part, attempts to persuade the reader that most emergency hospitalizations for adverse drug events in older adults are not the result of physicians prescribing inappropriate medications like those listed in the Beers criteria. Rather, the vast majority of hospitalizations are the result of a few commonly used medications, like warfarin, aspirin, plavix, and insulin. This would be an interesting finding, if it were true. Unfortunately, after reading this article I’m not sure it is.
Let’s start with the primary outcomes that the authors looked at – “hospitalization after an emergency department visit for an adverse event due to medications”. Here is a sampling of what they found:
- Over a quarter of a million (265,802) emergency department visits for adverse drug events occur annually among adults 65 years of age or older.
- Over a third (38%) emergency department visits for adverse drug events require hospitalization
- Nearly half (48%) of hospitalizations for adverse drug events involved adults 80 years of age or older
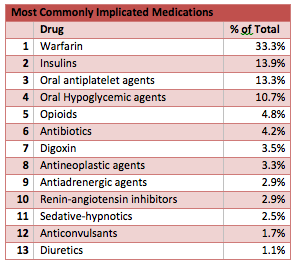
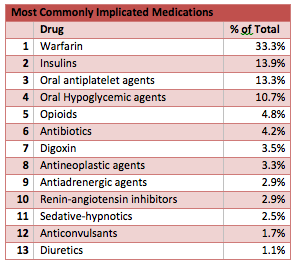
- Two thirds of the hospitalizations (67.0%) were the result of either warfarin (33.3%), insulin (13.9%), oral antiplatelet agents (13.3%), or oral hypoglycemic agents (10.7%)
Most of these adverse drug events were due to too much of a good thing. Bleeding due to too much warfarin. Hypoglycemia due to too much insulin. I thought this was nicely summed up by one comment the authors made
“The high numbers of hospitalizations for hypoglycemia from antidiabetic agents is consistent with mounting evidence of adverse outcomes from hypoglycemia and suggestions that current guideline and performance measures may not reflect optimal diabetes management for all patients.”
The secondary outcomes is where I thought the most interesting and dubious points of the paper laid waiting for me.
The secondary outcome that the authors looked at was hospitalization for an adverse event due to a medication currently designated as “high-risk” in the elderly by the 2011 HEDIS or “potentially inappropriate” by the 2003 update of the Beers criteria. The authors found that:
- Only 1.2% of hospitalizations for adverse drug events were attributed to HEDIS high-risk medications
- Only 6.6% of hospitalizations were attributed to Beers criteria potentially inappropriate medications.
- More than half of the hospitalizations for Beers-criteria medications involved digoxin
Does this mean the Beers criteria doesn’t matter, as long as you just don’t use digoxin? Absolutely not.
The authors state in their discussion that inappropriate prescribing only accounts for a small proportion of all admissions due to adverse drug events. However, the study only classified adverse drug events if an emergency department physician both identified and documented the adverse drug event.
What this study may actually tell us is that emergency physicians are really good at picking up not so subtle hemorrhages due to antithrombotic and antiplatelet agents, but they are more than likely not so good at picking up events like drug induced delirium. These types of adverse events from “inappropriate medications” are more likely to be diagnosed during the course of the hospitalization, or not at all.
Like the medical practice clinic that tries to get all their elderly diabetic patients to a goal Hgb A1C less than 7, the authors fall into the trap of doing too much with a good thing. This study gives good evidence that serious adverse events are common, and that the older you are, the more likely they will occur. Trying though to downplay the significance of inappropriate medication usage in the elderly just isn’t warranted given the limitations of their study.
by: Eric Widera



