

This is the third post in a series on copyright in medicine. We started off the series with two posts. The first discussed the importance of a NEJM article advocating for the greater use of copyleft licenses in medicine. The second detailed the dubious copyright infringement claims by the authors and owners of the mini-mental state exam. This last post in the series is a call for help maintain a bare minimum of open access to taxpayer funded research.
 A new Association of American Publishers (AAP) backed bill titled the “Research Works Act” is threatening the currnet National Institutes of Health (NIH) public access policy. The current NIH policy requires that all final peer-reviewed journal manuscripts that arise from NIH funds be submitted to PubMed Central upon acceptance for publication, and that these papers are accessible to the public on PubMed Central no later than 12 months after publication.
A new Association of American Publishers (AAP) backed bill titled the “Research Works Act” is threatening the currnet National Institutes of Health (NIH) public access policy. The current NIH policy requires that all final peer-reviewed journal manuscripts that arise from NIH funds be submitted to PubMed Central upon acceptance for publication, and that these papers are accessible to the public on PubMed Central no later than 12 months after publication.
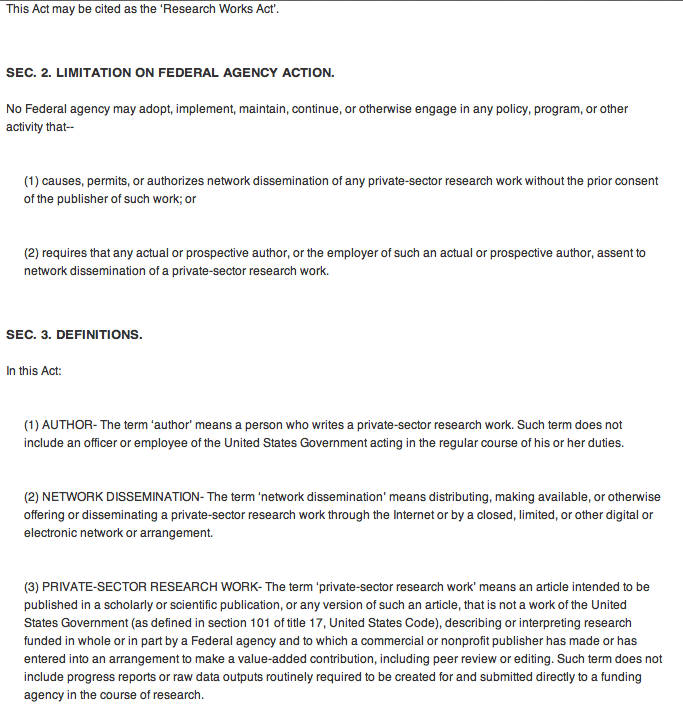
Despite an overly restrictive period of up to 12 months before making these works open to the public, Representatives Carolyn Maloney (D-NY) and Darrell Issa (R-CA) have decided to move forward with a bill that would effectively end open access to work funded by the federal government. The language of the bill is simple in its destructive power:
“No Federal agency may adopt, implement, maintain, continue, or otherwise engage in any policy, program, or other activity that:
(1) causes, permits, or authorizes network dissemination of any private-sector research work without the prior consent of the publisher of such work;
or
(2) requires that any actual or prospective author, or the employer of such an actual or prospective author, assent to network dissemination of a private-sector research work (i.e any non-governmental agency like a university).
Many journalists and bloggers have been up in arms over this issue. Major outlets including Scientific American, WIRED, and the Atlantic, have had articles lambasting the bill. So, what can be done? Michael Eisen from UC Berekely said the following in his blog post:
“It is inexcusable that a simple idea – that no American should be denied access to biomedical research their tax dollars paid to produce – could be scuttled by a greedy publisher who bought access to a member of Congress.” [Referring to political contributions that Dutch publisher Elsevier made to Rep Maloney]
He goes on to urge his readers to:
“call/write/email/tweet Representative Maloney today, and tell her you support taxpayer access to biomedical research results. Ask her why she wants cancer patients to pay Elsevier $25 to access articles they’ve already paid for. And demand that she withdraw H.R. 3699.”
By far the easiest thing anyone reading this post can do is to start off by tweeting Rep Maloney at either @RepMaloney or @CarolynBMaloney. I would also strongly encourage you to tweet Rep Issa at @darrellissa, as he proudly proclaims himself to be for “an #OPEN, accessible & uncensored internet” (makes you wonder why he proposes cutting off open access to journal articles).
Deevy Bishop, from BishopBlog, takes it one step further with a call to arms for her academic colleagues:
“We provide the articles for Elsevier journals, and we do a lot of unpaid work reviewing and editing for them. None of us wants to restrict our opportunities for publishing, but these days there are a lot of outlets available. When deciding where to submit a paper, I suspect that most academics, like me, take little notice of who the publisher of a journal is. I focus more on whether the journal has a good editor, my prior experience of publication lags, and whether Open Access is available. But as from now, I shall include publisher in the criteria I adopt, and avoid Elsevier as far as I can. Also, if asked to review for a journal, I’ll check if it is in the Elsevier stable, using this handy website, and if so, I’ll explain why I’m not prepared to review. I suggest that if you are as annoyed as I am by this story, you do likewise, and refuse to engage with Elsevier journals.”
I probably wouldn’t go as far as Deevy Bishop and I don’t think it is fair to single out Elsevier, but it does make me think of all the free labor that I willing give to these journals. A similar option is to take a “don’t peer-review articles from non-open access journals” approach as seen in this letter by Michael Ashburner posted on Casey Bergman’s blog.
Lastly, you can make your voice heard also to the the National Science and Technology Council’s Task Force on Public Access to Scholarly Publications. There is a Request for Information (RFI) on the Federal Register’s website that closes on January 12 (ignore the date on the website, the deadline was extended). This is not part of the bill, but it is another way to get your voice heard.
If you don’t know what to say for the RFI or in the letters to your representative, look at this link from the Provost of Harvard University, Alan M. Garber. Alternatively, you can also just ask for the bare minimum of open access protect as suggested by Stevan Harnad:
(i) the fundee’s revised, accepted refereed final draft
(ii) of all refereed journal articles (including refereed conference articles) resulting from the funded research must be
(iii) deposited immediately upon acceptance for publication
(iv) in the fundee’s institutional repository.
(v) Access to the deposit must be made gratis OA (online access free for all) immediately (no OA embargo) wherever possible (over 60 % of journals already endorse immediate gratis OA self-archiving).
By Eric Widera (@ewidera)
Addendum: for an excellent round-up of blog posts on this subject go to John Dupuis’ blog.



