A new survey commissioned by the California HealthCare Foundation gives some great insight into the attitudes and experiences that Californians have with death and dying. Thesurvey, conducted by Lake Research Partners and the Coalition for Compassionate Care of California, polled a representative sample of 1669 adult Californians including 393 respondents who lost a loved one in the past 12 months. The results can be summarized as follows:
Californians Want to but Don’t Put their Wishes in Writing
This survey shows that people when asked, actually want to discuss and plan ahead regarding end of life issues.
- Approximately 45% state that it is very important to put end of life issues in writing, followed by 37% somewhat important, 12% not to important, 4% Not at all important and 1% refused. However, only 23% have put it into writing, 76% have not and 1% refused.
- When asked if a loved one was seriously ill, would you want them to fill out a POLST form so that you would be clear about what he or she wanted 41% definitely, 30% probably, 21% maybe, 2% probably not, 2% definitely not, 1% refused.
Californians Want to But Don’t Discuss their Wishes with Their Doctor
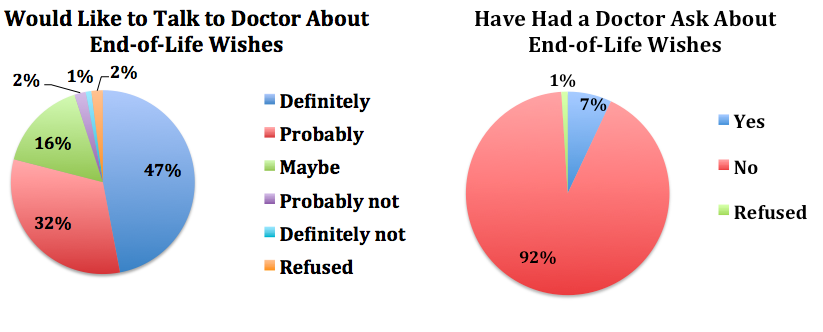
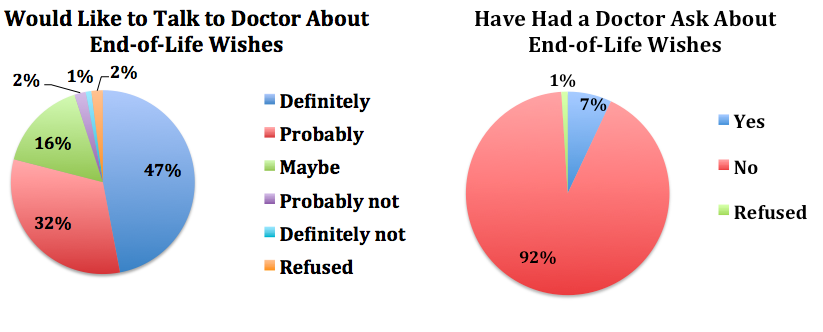
- When asked if you were seriously ill, would you like to talk with your MD about your wishes for the medical treatment toward the end of your life: 47% definitely, 32% probably, 16% maybe, 2% probably not, 1% definitely not, 2% refused.
- When asked have you ever had your doctor ask you about your wishes for medical treatment at the end of your life 7% yes, 92% no.
- When asked more than 4/5 Californians say reimbursing physicians for talking about end of life treatment options is a good idea.
- When asked 70% said they want to die at home, when in fact: 32% die at home,42% in the hospital, 18% nursing homes.
- The majority of those surveyed, 66% state they want to die a natural death, while only 7% state they would want all possible invasive treatment to attempt to prolong life.
Just checking in what does all of this data actually tell us so far:
- Patients, as consumers of health care, as a service based industry, are not receiving what they want.
- They would support a system that actually delivered what they wanted by trained professionals with paid reimbursement. This would include discussions regarding end of life care treatment options.
As shown in the article published by Alexi Wright and colleagues, end of life discussions are associated with No increase in patient depression or worry, improved patient and caregiver quality of life, decreased CPR, ICU admissions, earlier hospice referrals, less care giver depression. More aggressive therapies make no difference in mortality and worsen patient quality of life.
In essence we no longer have a choice as ethical health care professionals. Numerous studies and our personal experiences testify to the fact that excellent evidence, based, ethical patient care involves educating patients and their caregivers about what treatment options exist and what the potential outcomes are realistically.
In California not only ethically, but legally pursuant to California assembly bill 2747, effective January 2009, if a physician makes a diagnosis that a patient may have less than one year less to live they are ethically and legally obligated to offer to inform patients of all of their health care treatment options. This includes but is not limited to the right to forgo invasive treatment options and chemotherapy, and to elect symptom and dignity based treatments consistent with palliative based care.
Therefore ethically, legally, practicing evidence based medicine, consistent with our patient’s health care wishes, in concordance with the Patient Self Determination Act, they must be offered an opportunity to be informed of ALL of their treatment options. Our patients want to discuss this with us. Our medical system, Medicare is at a breaking point because as a profession we are not talking and listening to our patients. Therefore, this perpetuated dysfunction through lack of communication leads to patient, family, and health care professional suffering. There is no longer a choice, these discussions must occur! For physicians who are not ready training must take place, if they are unwilling they must offer to refer their patients to someone who is.
We know that the involvement of trained nonphysicians can in fact increase advance directive completion and facilitate them being readily available in the electronic medical record. This model was demonstrated in La Cross Wisconsin with the Lutheran Gunderson Medical Foundation (J Am Geriatr Soc 58:1249-1255, 2010). As this model is adapted and implemented across large health care systems patients’ health care choices are respected. After implementation these preferences were consistent with treatment decisions 99.5% of the time.
This is the end, but also this is just the beginning as we embark on a more humane, patient centered practice of the art and science of medicine.
By: Gideon Sughrue



