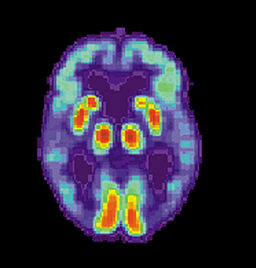
Last week the NY Times story on a new scan that identifies Alzheimer’s in the brain caught my eye, and probably caught yours too. What is the benefit of this test, wondered my colleague Alex Smith in a recent Geripal post, and is it worth the cost?
What is the value of “knowing for sure — period”?
I can’t say I know the answer for sure, but I do know that the period of uncertainty is hard on most families when we work up early cognitive impairment in the outpatient setting. (It usually lasts for months, if not longer.)
I also know that for geriatricians in outpatient clinical practice, the diagnostic question isn’t just “Is it or isn’t it Alzheimer’s?” It’s also:
- What’s causing this cognitive impairment?
- Is it dementia (of any stripe)?
- Are there any additional factors making the cognition worse? (As in: medications, medications, and oh yes, medications. Benzos and anticholinergics, I’m talking about you.)
The new brain scan, obviously, doesn’t answer many of these questions, nor does it directly lead to better dementia care for patients and families.
Still, I think that decreased period of uncertainty might be valuable, especially when I think about how the process of diagnosing early dementia usually goes. (I wrote about my experience of this process in more detail on the Geritech.org blog this week.)
So although usually I’m a less-is-more kind of clinician, I find myself conflicted about the scan.
Would I order it? Maybe.
What about the rest of you? I’m especially eager to hear thoughts from the other clincians who are diagnosing dementia in the outpatient setting.
by: Leslie Kernisan



