Bree Johnston, a true believer in geriatrics and palliative care, contributor to GeriPal, and erstwhile colleague at UCSF, recently returned to give grand rounds. She said that while in Scotland, she had the opportunity to observe geriatrics and palliative care teams. Bree previously posted many of her observations on the blog hereand here.
One thing I want to highlight about her experience was the contrast in what clinicians considered vital information about patient’s approaching the end of life in the UK. Their PPD status. What, you say, do they have severe outbreaks of tuberculosis among the dying?
No, PPD stands for Preferred Place of Death. They actually ask patients about their preferred place of death as part of the advance care planning process, document it, and make a big deal about trying to get the patient to that setting as death approaches.
This is remarkable! In the US the subject often comes up in the research literature, as in something like, “Most patients prefer to die at home but a majority die in institutions like hospitals and nursing homes.”
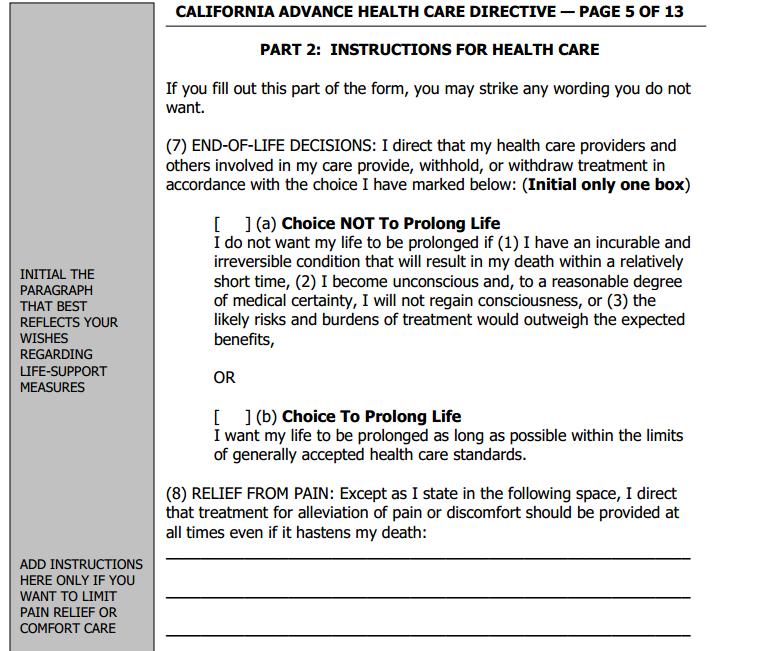
But we do not routinely as a health care system include preferred place of death as a part of advance care planning, or as a goal for care as patient’s health deteriorates. Preferred place of death is not captured on most advance directive forms (see picture). We sometimes ask in palliative care, but not routinely. It’s certainly a far cry from how code status is treated in the US: we’ve put it on a pedestal. Code status is now routinely assessed during hospital admission, once by the night float admitting the patient, then again in the morning by the day intern, and confirmed again later by the attending. Much-to-do about a little chest thumping, and arguably no where near as important as getting dying patients who want to be home, home.
Note: I was also reminded of preferred place of death while browsing all-things-palliative, a terrific compendium and calendar of, well, all things palliative! I immediately found a link to an interesting study finding that 70% of Albertans prefer to die at home.
Canadians – love ’em; married one.
by: Alex Smith



