 |
| From the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention |
It has been over three decades since the first cases of AIDS were observed in the United States, and in one month we will be marking the 30th anniversary of dual publications in Scienceattributing a novel retrovirus as the potential cause of AIDS.
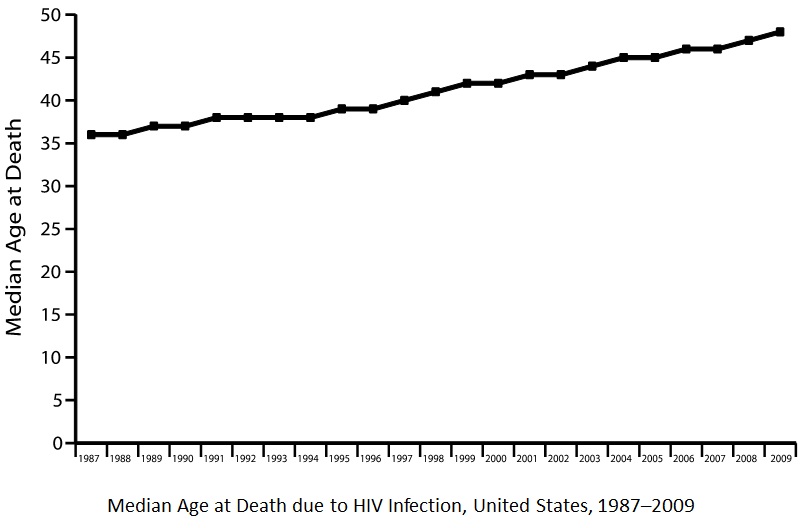
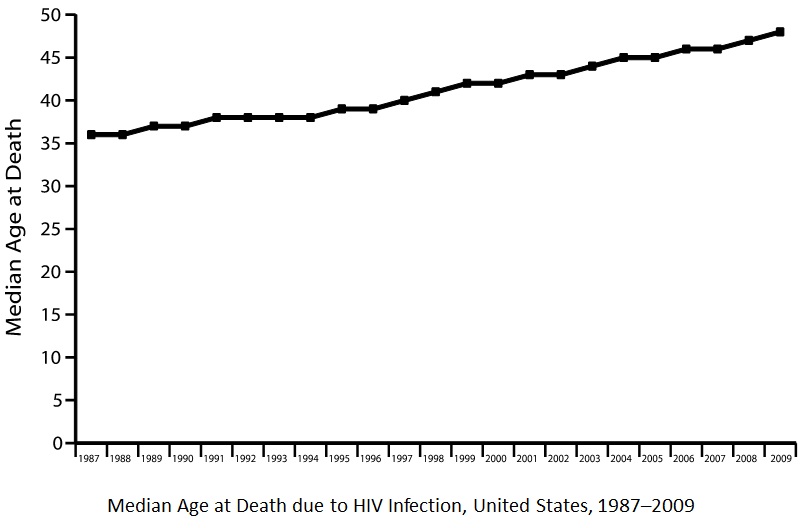
Since this time, and in large part due to the development of antiretroviral therapy, mortality due to HIV & AIDS has significantly decreased, so much so that it is now considered a chronic rather than an acutely fatal disease. With these changes, HIV is also now becoming a disease of the elderly. By 2015, half of HIV positive individuals will be older than 50 years of age.
This is the background to what I consider one of the most important review articles in JAMA this year. Starting off with a case of a 74 year old who was diagnosed with HIV in 1984 (when AIDS was almost a uniformly fatal disease) the authors, Meredith Greene, Amy Justice, Harry W. Lampiris, and Victor Valcour, walk us through the prevention and management of HIV in Advanced Age.
Here are a couple issues presented in the article that should make this a must read for any provider caring for older adults (you can read the entire manuscript here):
Under-diagnosis: There is a delay in the diagnosis of HIV due in part to common misconceptions that HIV is a disease of the young and that older adults aren’t at risk because they don’t have sex (or at least we dont ask about it.)
Screening: Age as a cut off for screening is changing. Because of shifting demographics seen in HIV infections, routine opt-out screening is now recommended regardless of age.
Antiretroviral Treatment: CD4 counts should not change the decision of when to initiate antiretroviral therapy. In the US, antiretroviral therapy should be started in all older patients regardless of CD4 counts.
Psychosocial Care Matters: Older HIV-positive adults are at risk for social isolation, which has been shown to negatively impact health outcomes (see here)
Prognostication: Patients overall goals and life expectancy should play a role in decisions around health care maintenance and prevention in this population (and they included a link to ePrognosis!)
Advance Care Planning & Palliative Care: Discussions and documentation of end-of-life preferences need to occur more frequently and Palliative Care can play an “emerging role in improving quality of life” in these patients
The review also does a beautiful job in helping clinicians understand how specific antiretrovirals are chosen in older HIV positive adults and common drug interactions between antiretrovirals and other medications.
To wrap things up, I’ll end with a quote from the article on where we need to be going as a field:
Optimal models of care must be identified—with HIV specialists, primary care clinicians, and geriatricians working together to make successful aging for this population achievable.
Well said!
by: Eric Widera (@ewidera)



