In April, the Food and Drug Administration (FDA) approved florbetapir F-18 (Amyvid) PET scans to identify areas of accumulation of amyloid plaques. Centers for Medicare and Medicaid Services (CMS) though has yet to allow reimbursement for amyloid PET scans for the evaluation of dementia outside of clinical studies, citing insufficient evidence that it improves health outcomes for Medicare beneficiaries.
The CMS decision is strongly opposed by Eli Lilly and its subsidiary Avid Radiopharmaceuticals, the makers of Amyvid. The Alzheimer’s Association also was “disappointed” by the CMS decision, stating that there was “clear, scientific consensus recommendations by the Association and the Society for Nuclear Medicine and Molecular Imaging (SNMMI) regarding appropriate, limited coverage, only in specific populations.”
So who is right? CMS? The Alzheimers Association? The Association and the Society for Nuclear Medicine and Molecular Imaging (SNMMI)? Eli Lilly? What about Ezekiel Emanuel? He just wrote a wonderful piece in theNY Times this weekend recommending that we should not “waste a lot of money on a test that really doesn’t help” due to the poor test characteristics of the scan and the anxiety that it can create. Given all these voices saying different things I’d like to throw my own take on the subject:
Eric’s 5 Point Summary of the Evidence for Amyloid PET Scans
1. Evidence Base for its clinical utility: poor.
- JAMA Internal Medicine just published an exellent review on the subject, which highlights the “extremely limited data with which to evaluate the clinical utility of amyloid PET.”
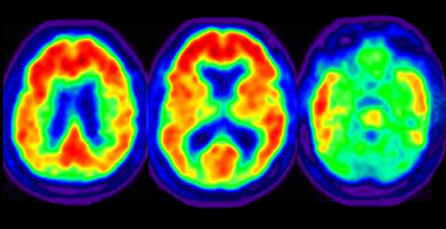
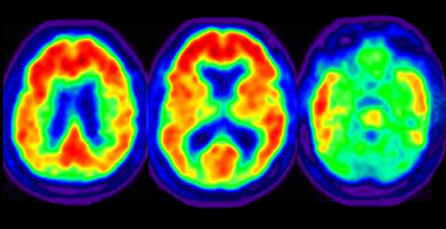
2. Ability to detect amyloid in the brain: great!
- There are some good studies demonstrating amyloid PET is accurate in detecting amyloid in the brain if the scan is read by well-trained interpreters. Unfortunately, there isn’t really evidence of what this training should consist of as the studies showing accuracy are using 3-5 very well trained physicians in academic centers per scan. Also of note, detection of amyloid is very different than diagnosing Alzheimer’s disease (more on that below)
3. The clinical usefulness of a positive test: unclear except in the elderly where it probably isn’t so good.
- The FDA-approved label for Amyvid states that a positive scan does not confirm the diagnosis of AD or other disease. Why? Amyloid plaques can be found in about a third of cognitively normal older adults as well as in other diseases. Furthermore, the older you are, the more likely you are to have amyloid in the brain even if you don’t have any cognitive impairment, significantly decreasing the positive predictive value of a amyloid PET scan. And with every diagnostic test, its the positive predictive value that really matters.
- So what does a positive test really add? There is somewhat soft evidence from a study by Doraiswamy that in the MCI population a positive amyloid PET may increase the risk for progression to clinically diagnosed Alzheimer’s disease in individuals with mild cognitive impairment. However, based on this study, 29% of those with positive scans progressed to clinically diagnosed AD compared to 10% of those with negative scans. In real life terms, what does a 19% difference really mean to a patient? Are they really going to do something different based on a 10% versus a 29% chance of developing Alzheimer’s disease?
4. The clinical usefulness of a negative scan: better given given the high sensitivity to amyloid pathology of the scan (still uncertain though)
- A negative scan means that you likely don’t have many amyloid plaques in your brain, which also means you probably don’t have Alzheimer’s (at least for now). However, based on the last study I mentioned on MCI, there was still a 10% conversion to clinically diagnosed Alzheimer’s disease in those with negative scans. Also, a negative scan doesn’t really help in figuring out what is causing the impairment other than it’s not likely Alzheimer’s. Finally, there are no good studies to suggest that a negative test changes in subsequent clinical management or whether any changes in management would produce net health benefits to those that really matter: patients and families.
5. The usefulness in prognosticating: unknown
- Again, based on the JAMA Internal Medicine article discussed above, there is no evidence to suggest that the test can be used to accurately predict the risk or the timing of progression of mild cognitive impairment.
Conclusion Based on the 5 Points
Amyloid PET scans: not ready for prime time. Good call CMS.
by: Eric Widera (@ewidera)



