I’m simultaneously a behavioral researcher, an ethicist, and a
hopeless Facebook addict, so I’ve been thinking a lot about last week’s
controversial study (Kramer
et al, PNAS 2014) in which researchers manipulated the emotional content of
689,003 Facebook users’ News Feeds. In summary, users who saw fewer of their
friends’ posts expressing negative emotions went on to express more positive
and fewer negative emotions in their own posts, while users who saw fewer posts
expressing positive emotions went on to express more negative and fewer
positive emotions in their posts.
This provides evidence for “emotional contagion” through
online social networks—that we feel better when exposed to other people’s
positive emotions, and worse when exposed to negative emotions. This finding
isn’t obvious, since some
have suggested that seeing other people’s positive posts might make us feel
worse if our own lives seem duller or sadder in comparison.
The journal and authors clearly did not anticipate a wave
of online criticism condemning the study as unethical. (Full disclosure: one
of the authors is also a researcher at UCSF, though I don’t think I’ve ever met
her.) In particular, the authors claimed that participants agreed to Facebook’s
Data Use Policy when they created their Facebook accounts, and this constituted
informed consent to research. Looking at the Common
Rule governing research on human subjects, it’s clear that the requirements
of informed consent (including a description of the purposes of the research, expected
duration, risks/benefits, compensation for harms…) are not met just because
subjects click “Agree” to this sort of blanket terms of use. There are exceptions
to these requirements, and some people have suggested that the research could
have qualified
for a waiver of informed consent if the researchers had applied for one. I’m not so sure about that argument, and in any case the researchers hadn’t.
While the online discussion about this study has been
fascinating, I think there are a few points that haven’t
received as much attention as I think they deserve:
1. This controversy
is taking place against a backdrop of more critical scrutiny of informed
consent among ethicists.While bioethicists in general have traditionally
advocated strong informed consent requirements in the name of participant
protection and self-determination, in recent years there has been an opposite
trend emphasizing that such requirements are burdensome and may inhibit
important research. Last year we saw a controversy over a neonatal ICU clinical
trial, in which many
experts criticized
regulators’ strict interpretations of informed consent. More recently, some prominent figures
have suggested that informed consent requirements in medical research should be relaxed,
particularly for “big data” studies made possible by electronic medical records
and coordinated health systems. Much like with the Facebook study, these
researchers and ethicists believe that new technologies hold promise for new
ways of conducting research to promote health, and worry that these
possibilities may be closed off by our existing ethical frameworks.
2. What’s “research”?One irony
of this controversy is that Facebook manipulates users’ News Feeds all the time—they
don’t show you everything that your friends post, but use a filter that they’re
always tweaking “in the interest of showing viewers the content they will find
most relevant and engaging.” (In other words: so that you’ll keep coming back
and they can show you ads.) These tech firms take a relentlessly empirical
approach to everything. Google once ran 41 experiments to
figure out which
shade of blue made users more likely to click on ads.
These activities aren’t categorized as research falling under
the Common
Rule, as typically construed, because they’re not designed to develop or
contribute to generalizable knowledge. So, e.g., if Facebook had a purely
internal purpose for figuring out how to manipulate users’ emotions by
adjusting the News Feed filter, this controversy wouldn’t have arisen. What
opens them up to ethical criticism here is that they tried to answer a more general
scientific question and published their findings in PNAS.
As others have pointed out, this division creates weird
disincentives. Experiments on Facebook users to improve Facebook’s own
processes and make more money don’t receive this level of scrutiny, but experiments to
answer general questions (and that are publicized in scientific journals) do.
But the risks to subjects are probably greater in the first case, since Facebook
will keep those studies and findings proprietary, and the social benefits are
smaller.
3. Social
media and technology are creeping us out.I agree with the
critics of the study that it didn’t meet existing requirements for informed
consent in research; however, I don’t think that’s why people have responded to
the story as they have. As in most cases, “the scandal isn’t what’s
illegal, but what’s legal.” In other words, what many of us really want to know
is: what other experiments are Facebook/Google/Apple/Amazon/Samsung running on me that they’re
not required to tell me about?
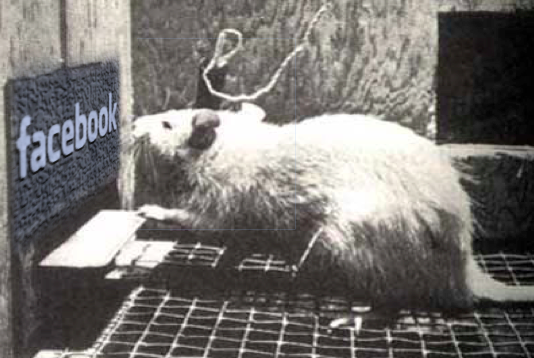
Like many people, I have complicated and ambivalent feelings
about my dependence on these technology giants. As a researcher, I think that
these feelings are a defining feature of our modern lives, and would be worthy topics for further empirical study. In a sense, the broad outcry
over this study is an illustration of why such research is so important, though
I worry it will have the unintended result of making future academic-industry
collaborations in this space less likely.
by: Winston Chiong



