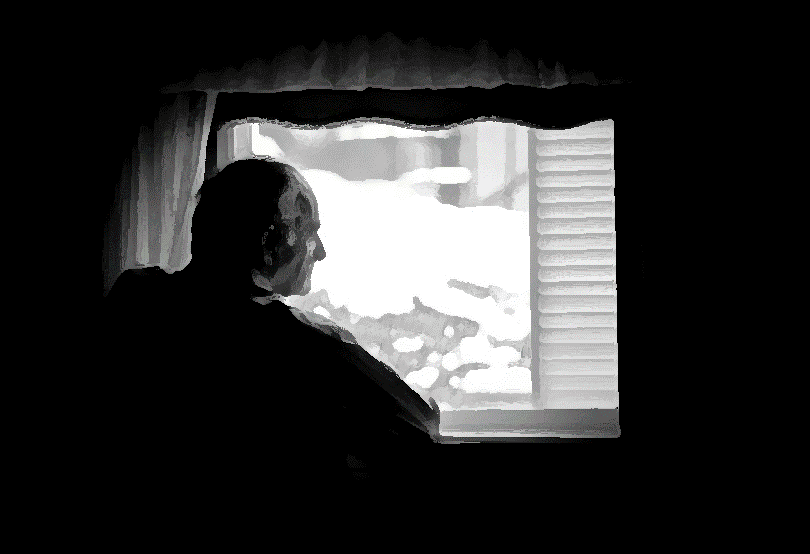
Have you ever had a patient at home who was in need of dental care? Perhaps they were receiving hospice services or maybe they were just discharged from the hospital not on hospice, but still too frail to get to the dentist. Of course the focus is often on the medical issues, yet the most significant issue was broken rotted teeth, which made oral intake nearly impossible without pain. Clearly, the answer here is not opioids for pain control, but rather to take care of the root problem: access to dental care.
Clearly dentists and their staff are not part of a hospice or palliative care IDT, but when you need them, boy do you need them. If the short case I outlined is not clear enough for you, I would really encourage you to read “Love” by Jean-Noel Vergnes, DDS, PhD recently published in the Annals of Internal Medicine (paywall). Written by a dentist in France caring for his wife who had a stroke and was desperately in need of dental care he himself could not provide, it illustrates the anguish of not being able to provide care you know someone needs.
“And little by little, it got difficult to clean her teeth with a toothbrush, too; she made little animal noises all the time, as if we were hurting her. So, it’s true that I didn’t take that much care of her mouth.”
Yet in the end there is a deep satisfaction when a dentist is found who will come to the home and provide the much needed care for his wife.
“Knowing that such a possibility existed made me change my mind. Actually, I’d always had this little voice in my head telling me that I wasn’t doing what was best for her, that I might be convincing myself that it was useless just because I didn’t have the strength to get on with it.”
Reading this story makes me reflect on the access to home visit dentists in my metro service area. When we need a dentist, the team works frantically to find someone willing to come out. So what are the barriers for a dentist? Is it malpractice insurance out of the office? Lack of access to the ever more complicated tools while in someone’s home? Lack of adequate reimbursement? Lack of time? I know many dentists do charitable activities in urban and foreign locations (usually for children), so I know the barrier is not likely to be a cold, uncaring heart. How can we as palliative care providers strengthen this relationship with dentists so the care is not needlessly delayed? The answers are likely complex and different in every community, and I know the answer is not theDentiDrillHome Dentistry Kit. Yet, I’m hopeful by asking this question of our great communities we might find a better answer together. Then maybe more people can have memories like this:
“She gave me a wonderful, broad smile. She was beautiful, so very beautiful. Ah, how can I put it? I knew that smile would be her last. I smiled back at her, savoring the moment . . . a moment that I couldn’t even try to describe. And that smile was, indeed, her last. I’ll remember it every day that I have left to live.”
by: Christian Sinclair, MD, FAAHPM – When he is not writing payback posts for GeriPal, you can find him over on Pallimed. (Post 1 of 4 in the World Series of Blogs payback)