GeriPal’s very own Alex Smith recently gave an absolutely fabulous “Ted-like” talk in which he made the statement that “prognosis needs to be a part of everyday medical care.” Unfortunately, as he so eloquently states in the video (which can be watched here), it isn’t always taken into account.
To dive a little deeper into the lack of prognosis in health care decision making, lets just take a look at cancer screening. Individuals with a limited life expectancy are exposed to all the immediate harms from a screening test, yet may not live long enough to see any of the benefit (the concept of lag-time-to-benefit). Yet, people with limited life expectancy still get these screening tests as evident by the following studies:
- A 75-year-old with severe comorbidities is twice as likely to be screened for colorectal cancer than a 76-year-old no comorbidities (click here for the article). This is despite that the knowledge that a healthy 76 year old is expected to live longer and is more likely to reap the benefits of screening. Why the big difference between 75 and 76 year olds? Probably because quality measures for colorectal cancer screening encourage screening up to the age of 75
- A study in the American Journal of Public Health examining mammogram use in older persons found that 18% of women with severe cognitive impairment had received a screening mammogram in the prior 2 years, despite an average life expectancy of 3.3 years (see this GeriPal post)
- Screening rates among patients with advanced, incurable cancer are only about a third to two-thirds of the rates of patients without cancer.
- Nearly half (48%) of primary care physicians would recommend breast cancer screening for those diagnosed with terminal lung cancer (click here for the article).
- In another study, about 45% of physicians said they would screen a 50 year old with unresectable lung cancer, a third would screen a 65 year old with unresectable lung cancer, and a quarter would screen an 80 year old with unresectable lung cancer
This is part of the reason that we created the ePrognosis: Cancer Screening decision support app to help guide conversations with elderly patients of whether to start, stop, or continue breast cancer and/or colorectal cancer screening. We recently updated it to give it a new look and feel, and for all you non-iPhone users, we are close to releasing a version that can be used on any mobile device (and yes, it will remain free of charge).
In Alex’s video, he leave the audience with a challenge, one that I’ll give to the GeriPal viewers as well. Alex asks the audience to use “ePrognosis once a week for the next month. See how it changes your perspective. See how it changes the conversations you have with your patients.”
by: Eric Widera (@ewidera)
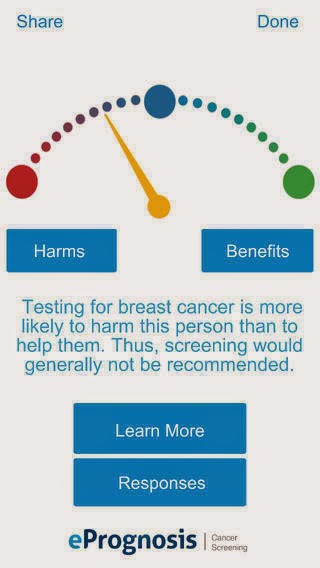 |
| The ePrognosis Cancer Screening app |



