By: Alex Smith, @AlexSmithMD
The following is a quote from an Emergency Medicine physician I interviewed for a study about palliative care in the emergency department:
I had 2 or 3 instances that involved a very angry
phone call from a primary care physician or an oncologist, who
understandably had had a several month conversation with this
patient, finally getting him to move to this DNR/DNI comfort
measure state, and then they come in and now we have them
intubated in the ICU, you know largely through
miscommunication. Part of the problem involves being able to
communicate effectively with people who know the patients
better—their primary care providers, their oncologists— but
who aren’t there at the ER at the time the patient comes in.”
This is a serious problem folks.
We spend a tremendous amount of energy working to help patients engage in advance care planning. We have pushed the envelope on getting patients to make plans in the outpatient setting, before they are seriously ill and having a “code status” conversation in the hospital with a doctor they’ve just met for the first time.
How often is all of this work for naught? How often do the best laid plans never make it to the hospital? How often is the patient picked up by the ambulance, seen in the emergency department, or transferred to the intensive care unit WITHOUT their POLST, DNR order, or advance directive?
I suspect this happens far more often than we recognize.
The failure to communicate advance care planning preferences can result in a tragic misalignment in care with preferences and goals. Such cases can be devastating for patients, caregivers, and clinicians alike.
Compounding the tragedy of these situations is the fact that this failure is in part entirely of our own devising. We have separate electronic health records at Kaiser, the VA, and the county hospital. Why? Because we encourage competition between electronic health record providers. As a terrible byproduct, we have a failure to communicate between health systems. And that failure is thrown into stark relief near the end of life, when someone receives the default pathway of resuscitation, intubation, and ICU transfer when they would not have wanted it.
It’s 2015 people! We should be able to solve this simple problem! And finally, someone has decided to do something about it.
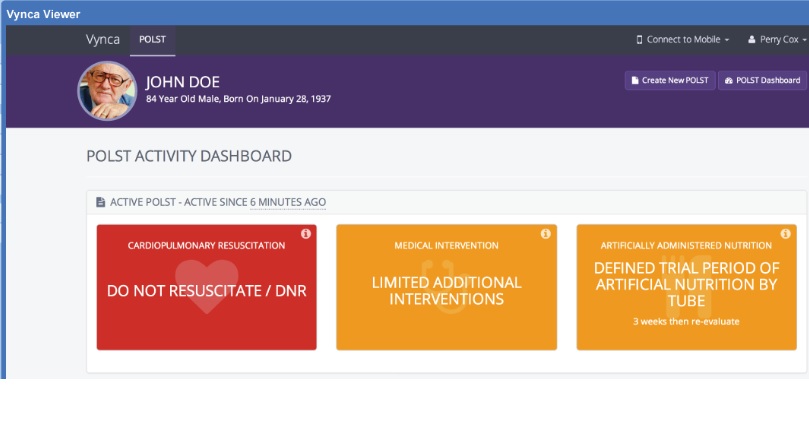
Ryan Van Wert and colleagues from Stanford have created an electronic POLST, or ePOLST. This is brilliant for several reasons:
1. Seamless integration into electronic health records across platforms
2. Secure cloud based storage of POLST information
3. electronic signature on an ipad or iphone of the POLST eliminates the need for ANY paper
What does this mean for our patients? It means clinicians will be able to easily check if the patient in front of them has a POLST, and read what it says. It means easy entry of POLST data, and ability to change it easily over time.
About damn time.
Notes:
1. They’re phasing in ePOLST in a big way in Oregon. See articles about the rollout of ePOLST here, here, and here.
2. Oregon is great because 1. They started POLST; 2. Best summer weather in the US; and 3. Best berries in the US).