by: Eric Widera (@ewidera)
“But one of the most sobering facts is that no current policy or practice designed to improve care for millions of dying Americans is backed by a fraction of the evidence that the Food and Drug Administration would require to approve even a relatively innocuous drug.”
Scott D. Halpern, M.D., Ph.D., NEJM
What? What??? Really? No current practice designed to improve care for dying Americans is backed by a fraction of the evidence to approve a drug? Are you kidding me? What about palliative care?
This is the second sentence of a NEJM article that was published today. While the intention of the article is actually good (more research is important in end of life care) the article completely misses the significant advances in palliative care over the last decade.
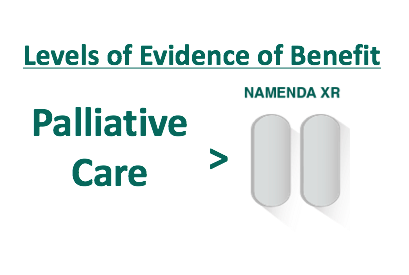
We do now have a growing evidence base for palliative care and now several randomized control trials on the impact that palliative care has on improving the care and outcomes of patients who are dealing with serious illness (1,2,3). I would argue that this level of evidence is not just a fraction of evidence, but is more compelling then data behind some drugs approved by the FDA (Namenda XR anyone?)
I’m still digesting this article and its key point that we should treat end-of-life care as we treat a drug approval process. While it makes a nice pithy statement, it misses points such as palliative care research is funded at a miniscule fraction that we fund research in other areas (Palliative care receives 0.01% of the National Institutes of Health budget).
Please read the article and let me know your thoughts. Anyone else disturbed by the message (I know I shouldn’t write when emotional so I may just be missing something here).
References
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. The New England journal of medicine 2010;363:733-42.
- Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014;383:1721-30.
- Bakitas M, Tosteson T, Lyons K, Dragnec K, Hegel M, Azuero A. Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J Clin Oncol 2015;33.



