
by: Danny Cox (@dannyMD)
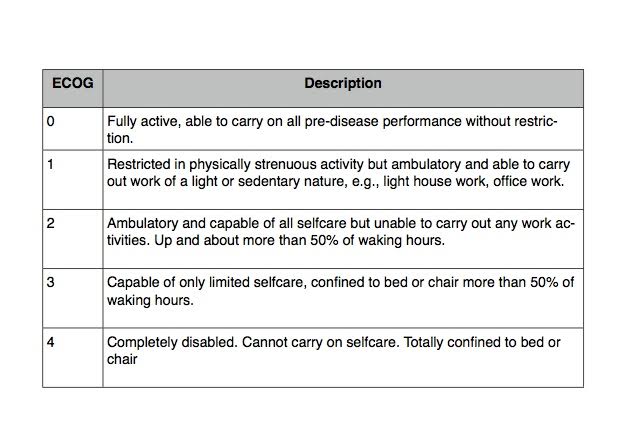
The goal of palliative chemotherapy for patients with terminal cancer is to prolong survival and improve quality of life. A major ongoing concern among many physicians is that chemotherapy given to those near the end of life might actually be doing more harm than good. The 2012 American Society of Clinical Oncology guidelines recommend against the use of chemotherapy for those with an ECOG score of ≥3 (ECOG is a graded scale of functional status; see table). The implicit assumption is that those with better functional status will be better able to tolerate chemotherapy and derive benefit.
An eye-opening new study entitled “Chemotherapy Use, Performance Status, and Quality of Life,” recently published by Prigerson et al. in the September 2015 edition of JAMA Oncology casts doubt on the perceived benefits of chemotherapy in terminally ill cancer patients even with good functional status and highlights the need for a more nuanced approach.
In this multi-center, longitudinal cohort study, 312 patients with progressive metastatic cancer with a life expectancy of ≤6 months with failure of at least 1 prior chemotherapy regimen were enrolled and followed prospectively until death. Significantly, half of these terminally ill cancer patients (50.6%) were receiving chemotherapy when enrolled in this study at a median of 4 months before death. And here’s the kicker: patients with good performance status at baseline (EGOG = 1), i.e. those most likely to “benefit” from chemotherapy, had worse QOL near death than those who did not receive chemotherapy. Patients with poorer performance status (ECOG ≥2) did not derive a QOL benefit from chemotherapy. Moreover, there was no survival benefit to chemotherapy in this study population.
So why is this happening? Why are our sickest cancer patients receiving toxic chemotherapeutics near the end of life when common sense, and now this new evidence, would dictate that there is limited benefit and even harm? One reason is that a physician, when faced with a patient in a terrible situation who is desperate to live, feels compelled to offer hope, to do something. It may be easier to write the next chemo order that the patient is requesting than to have a very difficult conversation acknowledging that a patient’s prognosis is limited and the treatments that have been tried have not worked.
Given this new evidence, physicians must have more candid conversations with their patients about the limited benefits and real risks of chemotherapy in terminal cancer. This way, patients and their families can make informed decisions about what is likely to happen rather than what they hope will happen. Medical education and professional development need to fill the gaps in communication skills to train our current and future oncologists to have these compassionate, courageous, and informative conversations. And together with their palliative care colleagues, oncologists must be armed with more tools in their proverbial tool belts like symptom relief and psychosocial support so that they can meaningfully offer something at that critical juncture when their terminally ill patient is crying for help and chemotherapy will not be effective.
A final take-away question introduced by this study: should tumor shrinkage or patient experience be the primary endpoint by which we judge the efficacy of any chemotherapeutic? Currently, most chemotherapy drug trials look at end-points like tumor size and time to progression of disease. Almost none examine QOL. The problem with the current end-point analysis paradigm is that you can make a tumor smaller, but the patient might not feel any better.
In fact, they sometimes feel worse.



