by: Jeffrey M. Levine MD, AGSF
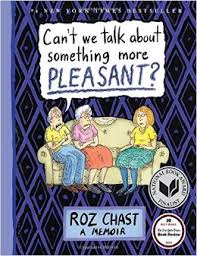
I had a chance to interview Roz Chast, the New Yorker cartoonist and best selling author of Can’t We Talk About Something More Pleasant? This bestselling graphic memoir is quite unique as it deals honestly with personal and emotional issues of caregiving for aging parents, and on the way covers many issues that geriatricians and palliative care specialists deal with on a regular basis. It is also now available in paperback.
Jeffrey: You are an artist known for your cartoons for New Yorker magazine, as well as your books that bring out the humor in everyday life. I am a fan of yours and it’s a pleasure to have this assignment from the Geriatrics and Palliative Care blog to ask you questions about your book.
Let’s talk about the title of your book. The title underscores a basic issue that geriatricians deal with on a regular basis – that is how to get an elderly person to face the difficult conversations of end-of-life choices. When you wrote this book did you expect that your graphic novel would have such wide application for so much of our aging population?
Roz: I didn’t think about that. I had no idea how or if it would apply to anyone else. I wrote it mainly for myself—so that I would remember them, and also the process of dealing with their final ten years or so, in greater detail than had I not written stuff down.
Jeffrey: You write with acerbic wit and at times hostility about doctors and hospitals. Your mother for example said that doctors have a “god complex” and hospitals are a place to die. You relate a harrowing anecdote about accompanying your parents on an ER visit with discourteous staff and endless waits. Do you think the average doctor, and our medical system, is prepared to deal with the problems of old age?
Roz: No, I don’t. We don’t deal with death in this society. We pretend it doesn’t exist. Crank up the Muzak and spray the whole topic with room freshener. I really hope that by the time I get “up there,” IF I get “up there,” there are better ways of dealing with what happens in those closing chapters. More help for the caretakers, should we be lucky enough to have them. And no weirdly-themed, infantilizing dinners in old-age facilities. I didn’t invent that detail in my book about the “Outer Space” themed dinner at the assisted living place my parents were in. So demeaning and depressing.
Jeffrey: You take the reader through placing your parents in assisted living, obtaining a home attendant, and placement in a nursing home. You describe a facility for the aged in Brooklyn as “depressing, torn carpet, dirty, flaking walls…” etc. As a geriatrician in the New York Metro area I know that places like this exist. There are also clean and well run places. What do you think society should do to improve conditions in our institutions for the aged?
Roz: I’m not a politician, a sociologist, an economist, or a geriatrician. All I know is that our society is organized to reward the top one percent of the top one percent with insane amounts of money. So, at the risk of sounding like a Socialist, I wish that somehow, we could all agree that this is nuts, and we have to spread the money around a little more equally. My parents saved up for their old age and were lucky enough to be in a non-disgusting facility. I don’t know what happens to people who didn’t.
Jeffrey: Your description of the aging process is achingly funny but startling accurate. Did you do any research on aging for your book apart from what you learned in the caring process?
Roz: None whatsoever. None needed. I had two textbook examples right in front of me, like anyone else who is taking care of a person or people who live to a very old age.
Jeffrey: Some of the things you write about, for example debridement of painful bedsores, a mass in your father’s chest, and a fistula in your mother’s abdomen are discussed in the context of palliative decision making but without directly using the term. You describe for example your own doubts on whether surgery is a humane idea if there was additional pain and poor choice of survival. As we progress in this century palliative care is becoming more common but my guess is that you did not encounter palliative care specialists when you cared for your parents. Do you think that a better presentation of palliative care principles through a specialist would have helped you and your parents through the process?
Roz: I think as palliative care becomes more normalized, it will be better for everyone. If my own final chapter involves palliative care , I am hoping to have access to psychotropic drugs. I might change my mind when the time comes, but I think about this a lot. Seriously, why not use the time to do some exploration of consciousness? I think there’s research being done on this topic—whether certain drugs like LSD, given in controlled doses and situations, can help people deal with the dying process.
——-
Jeff Levine is Associate Professor of Geriatrics and Palliative Care at the Icahn School of Medicine at Mount Sinai in Manhattan, and sees patients at the Center for Advanced Wound Care at the Mount Sinai Beth Israel Medical Center. Read his review of this book at: http://www.geripal.org/2015/05/insights-into-geriatrics-by-cartoonist.html



