by: Timothy Poore (@TimCPoore)
More than 90% of non-institutionalized people over the age of 65 in the United States receive health insurance through Medicare.(1) Of the money Medicare spends on individuals, it spends nearly one quarter in the final year of one’s life, and the majority of that money is spent on hospitalizations.2,3 With much talk during this election season about entitlement reform and the looming bankruptcy of Medicare, a study recently published in The Journal of Palliative Medicine is of particular interest, offering insight on how Medicare could save money by focusing on end-of-life care at home.
Cost Savings of Home Based Palliative Care
Dana Lustbader and colleagues conducted a retrospective study, comparing costs of care and resource utilization during the final year of life for patients who were enrolled in a home based palliative care program, and those who received usual care. All patients included in this study received their care from ProHEALTH Care (a multispecialty physician practice in the New York metropolitan area), died between October 1, 2014 and March 31, 2016, and had 12 months of continuous Medicare claims data prior to their death.
Here are some specifics of the Home Based Palliative Care Program used in this study:
- Staffed by 6 nurses, 2 social workers, 2 doctors, 1 data analyst, 3 administrative staff, and 12 volunteers
- Each nurse follows 90 patients on a team with a social worker and a palliative care physician
- Each patient gets approximately one home visit and two telephone calls per month with extra outreach as needed
- Program provides 24/7 telephone coverage by one of the program physicians
- Patients include homebound frail elders, those with advanced heart failure, COPD on home oxygen, metastatic cancer, or severe dementia
What did they find?
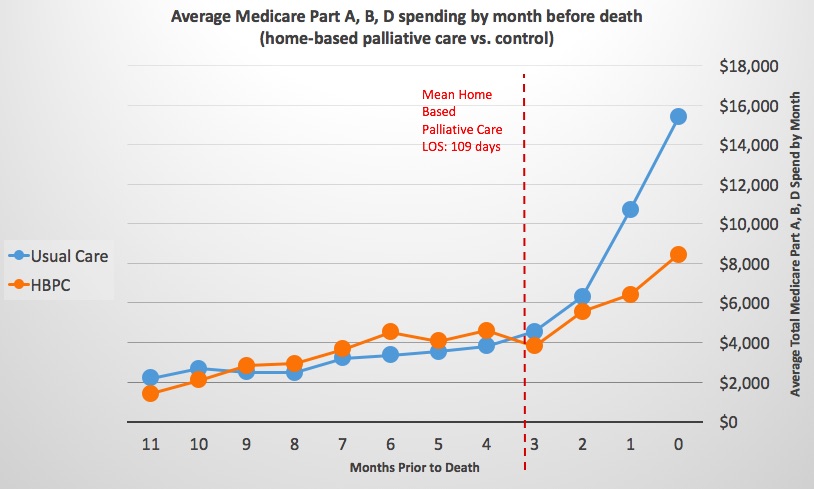
Of the 651 patients who died during the 18-month study period, 82 were enrolled in the Home Based Palliative Care Program and 569 received usual care. When comparing the 2 groups, the authors found that for those receiving Home Based Palliative Care:
- Medicare costs in the final year of life were $10,435 lower
- The cost per patient during the final 3 months of life was $12,000 lower (largely driven by a 35% reduction in utilization of Medicare part A)
- Hospital admissions were reduced by 34% in the final months of life
- Hospice utilization and length of stay on hospice were both significantly higher (35% and 240% respectively)
Lastly, they found that being on Home Based Palliative Care was associated with a very high likelihood of dying at home (87%) as compared with a national rate of 24% for all Medicare beneficiaries.
The Take Home
Nearly 90% of adults say that they would prefer to receive end-of-life care in their homes if they were terminally ill, yet only a small proportion of Medicare beneficiaries die in their homes.(2,4) This study shows that a home-based palliative care program can decrease unwanted hospitalizations, increase the chances of dying in one’s home, and improve utilization of hospice services, all with a significant savings in cost.
Hospital-based palliative care programs have been growing rapidly across the country, largely due to the mounting evidence of improved quality and costs savings. Maybe it is time we focus some of those expansion efforts on providing care for patients where they actually want it – in their homes.
Additional References
- US Department of Health and Human Services Administration on Aging. “A Profile of Older Americans: 2015.” http://www.aoa.acl.gov/aging_statistics/profile/2015/docs/2015-Profile.pdf
- Kaiser Family Foundation. Sep. 26, 2016. “10 FAQs: Medicare’s Role in End-of-Life Care.” http://kff.org/medicare/fact-sheet/10-faqs-medicares-role-in-end-of-life-care/
- Gerald F. Riley and James D. Lubitz, “Long-Term Trends in Medicare Payments in the Last Year of Life,” Health Serv Res 2010;45 (2): 565-76
- Joan M. Teno et al., “Change in End-of-Life Care for Medicare Beneficiaries,” JAMA 2013;309(5):470-77.