by: Eric Widera (@ewidera)
One out of every four people living in the United States will die in a nursing home. To say that access to palliative care is lacking for these individuals would be an understatement. What palliative care is delivered is too often limited to those who are eligible for and elected hospice care.
A study published in JAGS this weekgives us some of the best evidence so far that palliative care can be delivered in this setting, and is associated with less hospitalizations and burdensome transitions.
A Study of Palliative Care in the Nursing Home
The study authors looked at data from two palliative care provider organizations that were subsidiaries of hospice agencies in order to identify nursing home palliative care consultations in North Carolina and Rhode Island. Between the study years of 2005 to 2010, these two organizations were the only providers of palliative care consultations in the two counties in North Carolina and the six in Rhode Island where study nursing home were located. The data from these patients were then linked to Medicare and MDS data.
The authors compared this group to a propensity score matched group to control for factors such as age, gender, race, gender, cancer or dementia diagnosis, functional and cognitive impairment, recent hospitalizations, nursing home characteristics, and DNR orders.
.
Ok, What Did They Find?
The authors ended up comparing 477 nursing home residents who died between 2006 to 2010 with initial palliative care consultations within 180 days of death against 1,174 propensity score–matched controls that did not receive these consultations from the same nursing homes.
Residents with palliative care consultations had:
- Reduced hospitalizations in last 7 days of life, in last 30 days of life, and in the last 60 days of life
- Reduced ED visits in last 30, and 60 days of life
- Fewer burdensome transitions
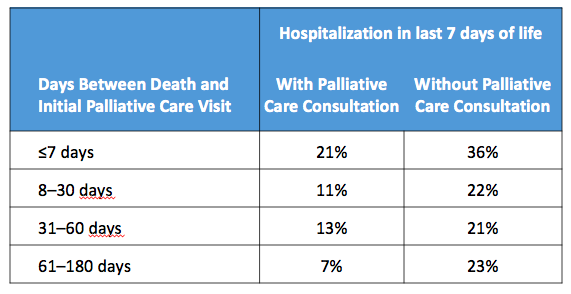
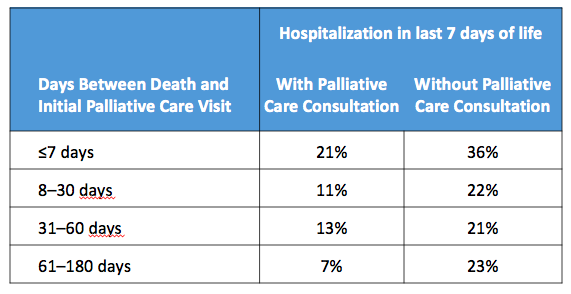
Furthermore, earlier admission to consultation programs was associated with lower hospitalization rates in the last 7 days of life.
Lastly, the adjusted Medicare expenditures in the last 7 days of life were significantly lower for residents with initial consultations in the last 30 and 61 to 180 days of life than for controls.
The Take Home
In a closely related article in JPSM, the same authors found that nursing homes introducing specialty palliative care consults experienced greater overall reductions in end-of-life hospitalization rates compared to nursing homes not introducing consults. Also, in another JAGS article, for every three nursing home residents that participated in an advance care planning intervention using specially trained nurses, two changed their documented treatment preferences.
Taking all of this data as a whole, it’s encouraging to see that palliative care can actually work in community nursing homes. I have to wonder though, how many of our palliative care trainees get any meaningful experiences in nursing homes in order to prepare them to give these types of consultations?




