“Never be the first to use a new descriptive term for older people nor the last to give up an old one.”
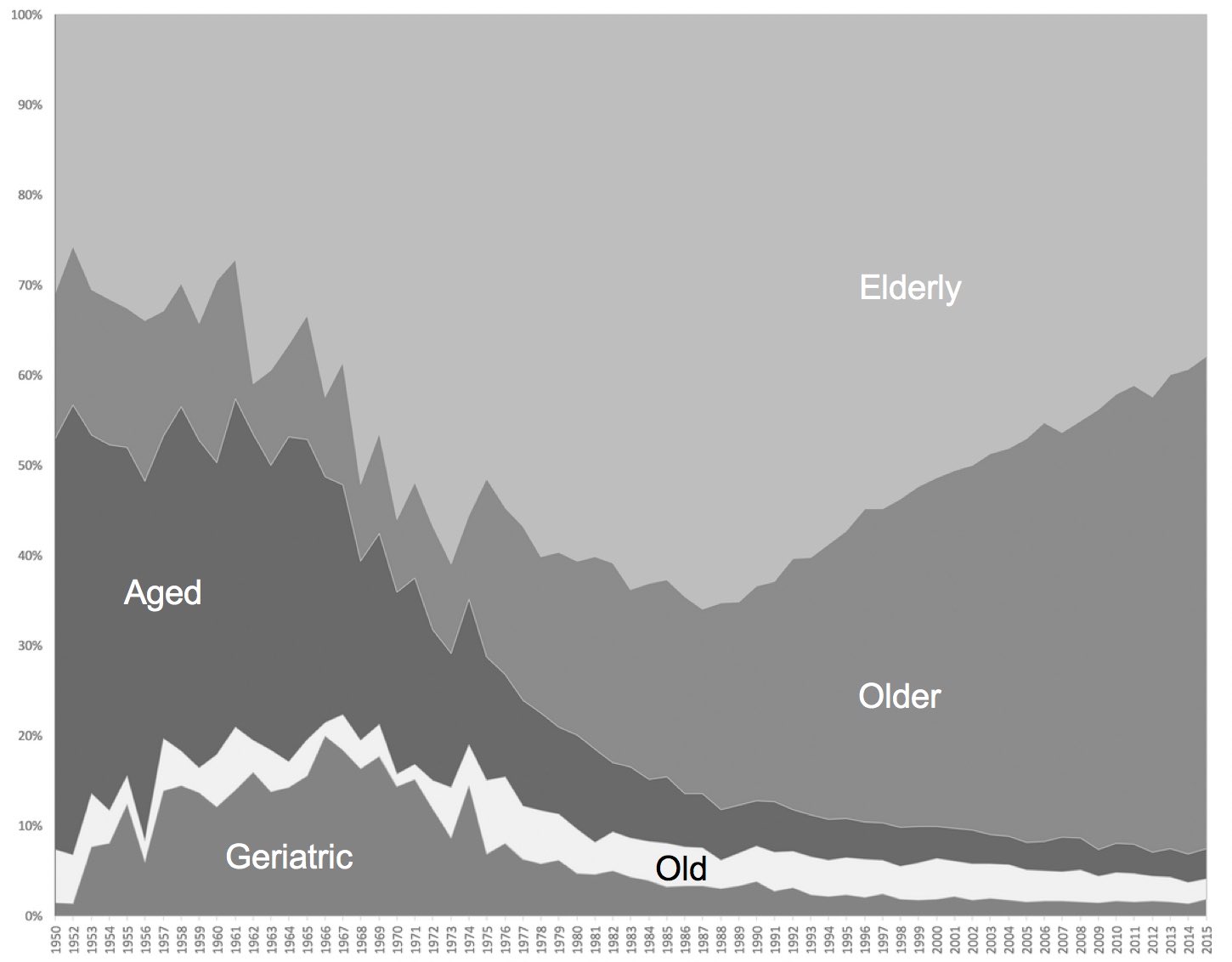
This is the advice given by Laura Morrison and colleagues in the discussion section of a fascinating new study published in JAGS this week. The authors looked at how “older people” are described in the English-language medical literature from 1950 to 2015. Specifically they looked at the use of the terms “geriatric,” “aged,” “old,” “older,” and “elderly” in Pubmed.
Here is what they found:
- We liked using the term “aged” in publications before 1961, but “aged” quickly lost its appeal over the next decade
- “Geriatric” became more common from 1955 to 1976 but again fell out of favor over the last couple decades
- “Elderly” peaked around the time of George Michael’s release of “Father Figure” (I’m not sure if there was a connection between the two)
- “Older” hit its low point in 1962 but boomed in use with the boomers, and is now our most popular term accounting for 55% of references
Alex Smith wrote about this topic in 2012, which garnered quite a bit of comments when he also advocated for the word senior (which was surprisingly lacking in this current study). In the end, there isn’t really a right answer as language continues to evolve.
So it I’ll end this post with a quote from the article that should give us pause for advocating for any particular word to passionately:
“The meanings of many words shift with time. Unfortunately, of the categories that linguists use to classify such semantic changes, “degeneration (pejoration)”—the acquisition of more-negative or more-disparaging connotations with time—best describes the changes of many words pertaining to older people.”
by: Eric Widera (@ewidera)



