I still clearly remember the first time I heard the name Rob Buckman. It was in fellowship when I was led to his book called “How To Break Bad News: A Guide for Healthcare Professionals” and what became the single most important mnemonic in my career as a medical educator: SPIKES. SPIKES not only gave me the language to break bad news to my patients, but also gave me a way help learners navigate some of the most difficult communication challenges in medicine.
Now, well over a decade later, I still use SPIKES every time I teach about breaking bad news, but I don’t think about Dr. Buckman much. That changed on my car ride home. I was gearing up to listen to one of my favorite podcasts, 99% Invisible, and up popped the title of the next episode “Breaking Bad News.” I paused for a second, thinking “what is a podcast about architecture and design doing talking about breaking bad news?”
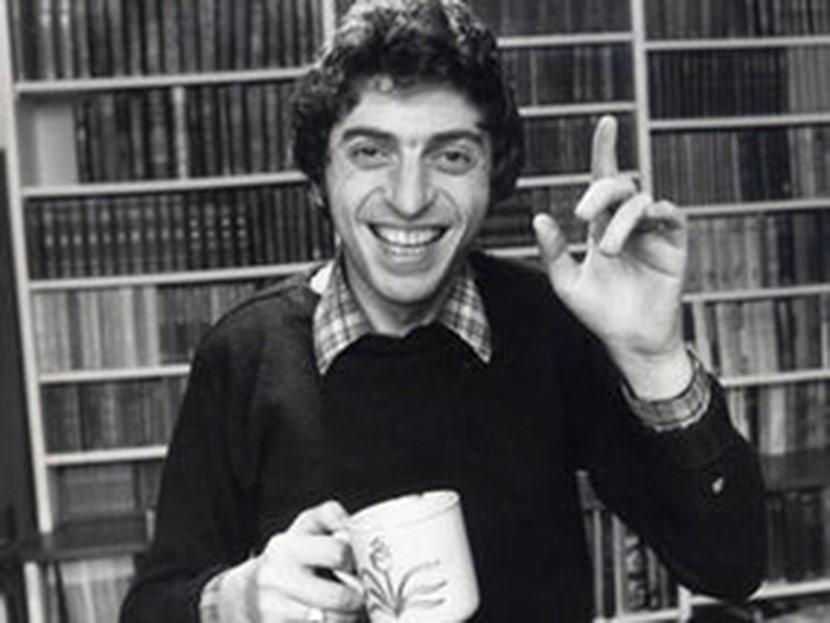
Well, the podcast was absolutely amazing and I highly recommend listening to it (and sharing it with trainees). I not only learned about the history of breaking bad news in medicine, I also learned a lot about the life of Rob Buckman. For example, Dr. Buckman was not only the granddaddy of breaking bad news, he was also a comedian. Take a look at these two clips of Dr. Buckman (and yes, that is the Monty Python Cheese Shop Sketch with John Cleese):
So, sit back, relax (unless you are driving), and walk down palliative care history lane. Maybe the next time you give a talk using the SPIKES mnemonic you may break into a British accent and ask for some Wensleydale.
by: Eric Widera (@ewidera)



