What’s the role of geriatrics and palliative care in the care of individuals with COPD? We talk this week with Anand Iyer, the lead author of this weeks JAMA IM article on this subject. It’s a little off from our ongoing COVID topics, but given that his along with his co-authors (Randy Curtis and Diane Meier) JAMA IM piece just got published, we figured now is the right time to highlight #PalliPulm.
What is #PallPulm? #PalliPulm is something that Anand Iyer founded, and is an online community of clinicians, investigators, patients, and others interested in the intersection of palliative care and geriatrics. Anand is also an Assistant Professor in Division of Pulmonary, Allergy, and Critical Care Medicine at the University of Alabama at Birmingham (UAB) and faculty at the Center for Palliative and Supportive Care at UAB.
Anands research on this subject has shown a lot of things, including that COPD patients are often referred too late to palliative care and hospice, pulmonologists often equate hospice with palliative care, there is high symptom and emotional needs in COPD patients, and that patients and family members feel palliative care should be integrated early on in the care of COPD. Here are links to some of these articles:
- A Qualitative Study of Pulmonary and Palliative Care Clinician Perspectives on Early Palliative Care in Chronic Obstructive Pulmonary Disease
- A Formative Evaluation of Patient and Family Caregiver Perspectives on Early Palliative Care in Chronic Obstructive Pulmonary Disease across Disease Severity
- End-of-Life Spending and Healthcare Utilization Among Older Adults with Chronic Obstructive Pulmonary Disease
We also talk about this podcast with David Currow on the use of opioids in dypsnea:
So take a listen and join the conversation at #PalliPulm!
by: @ewidera
Eric: Welcome to the Geripal Podcast. This Is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, who do we have on Skype today?
Alex: On Skype today we have Anand Iyer, who is assistant professor at the University of Alabama at Birmingham, who is in the division of pulmonary allergy and critical care. He also has an appointment in the center for palliative care at UAB, and he’s the founder of…
Eric: #Pallipulm.
Alex: #Pallipulm. We will talk more about that.
Eric: So before we talk about #Pallipulm, welcome to the Geripal podcast. Do you have a song request for Alex?
Anand: Yeah, it’s probably your first person from Alabama. I got to choose a song that came out of Muscle Shoals. Hopefully your audience knows about Muscle Shoal. Probably every hit from the 60’s came out of there, the same recording studio.
Eric: Never heard of it before.
Anand: Yeah, you got to, Google it. So Rita Franklin, Leonard Skinner, Rollingstones, everybody recorded there. So Land of 1000 Dances by Wilson Pickett. Let me see what you got.
Alex: All right.
Alex: (Singing).
Anand: Yeah awesome.
Alex: That is a jam.
Anand: That is a jam. That’ll get your two year old dancing right there.
Alex: That was a fun one.
Eric: That was awesome. I got the energy now. I don’t even need coffee.
Eric: So Pallipulm, what the heck is#Pallipulm? Is that a type of Berry?
Anand: Yeah, Pallipulm is an online community I started last year to clinicians, investigators, patients and caregivers to bring palliative care to people with chronic respiratory disease, and now it’s grown to be something worldwide. But if you’re a fan of Star Wars, I think Pallipulm is more of a higher state of being. It’s where you can bring the best of both disciplines into one person. So palliative care, pulmonary medicine. It’s a good side of the force. [laughter]
Eric: I love it.
Alex: Wait, that was an analogy about bringing together the good side and the dark side into one person or something like that. [laughter]
Anand: I don’t know about the dark side, but….
Alex: I was going to ask which is the light, which is the dark. It’s good. It’s good. [laughter]
Eric: And you’ve written a lot about this, and it focused a lot on… How did you get interested in this as a topic?
Anand: Like everything, it starts at the bedside. You could care for patients as a resident, we’ve all probably admitted dozens if not hundreds of patients with COPD exacerbations in the hospital or seeing them in clinic and find out that they have a lot of needs, not only extending for their own but to their family members. And as a fellow, I did more of that and saw that those needs were huge, and I was the one that was intubating them.
Anand: And so over and over and over and to a point where that gets to you psychologically, where you’re like, what’s going on here? They don’t know what’s happening in their disease course, and their utilization is high, coming to the hospital over and over. Plus they just have a really poor quality of life near the end of their lives, and they could really use palliative care but were never getting it. So I started out as a, made that a research career. A lot of my initial research was very clinical and things like pulmonary artery enlargement and Medicare samples, but I’m shifted into how does palliative care fit into this picture in the last few years.
Eric: And I can imagine there’s a kind of an analogy with heart failure in palliative care, in one way, when we think about heart failure specialists, some of the best symptomatic management for dyspnea and heart failure is really good heart failure management. I could see for the same thing, some of the best ways to treat dyspnea and COPD is really good COPD management.
Eric: So when we think about the needs for these patients, if we just focus on really good pulmonary care of their COPD to treat their dyspnea, do you really need another specialist involved in their care? Do we have all the needs met?
Anand: Big answer is no, we don’t. Dyspnea is just one piece of the puzzle. Yes, it’s one of the biggest pieces, but so is depression, anxiety, and inability to cope and prognostic awareness. These are all things that I’ve discovered in my own research, but that was the extend to the patient and their caregivers. So there’s a lot to offer from, not only palliative care, but geriatrics in the broader scope.
Eric: Yeah. Well, let’s talk about some of your research. So you did a study in Annals of ATS, American Thoracic Society. Looking at some of the needs for patients and family members, do you want to describe a little bit about kind of what you did there and what you found?
Anand: Yeah, that was a qualitative study of patients with moderate to severe COPD and their family caregivers. We had audio recording, semi-structured in depth interviews, and then conducted thematic analysis and discovered five major themes raised by patients and their caregivers. Those were coping with COPD, emotional symptoms, respiratory symptoms, illness understanding and prognostic awareness. But what was unique about that study was focusing on early palliative care, and that’s how to care long before the end of life.
Anand: Patients and their caregivers universally accepted the concept, although they had almost never heard of it. And these five themes of needs were shared across disease severity. So it wasn’t just something which is currently happening that you should wait until the end of life to do, rather you could start incorporating it in less severe COPD. And that’s been the whole crux of my research the last two years. Don’t wait until they’re on the vent in the ICU to start palliative care.
Eric: And when you talk about early palliative care, what were you talking about there? Were you’re talking about early identification of palliative care needs in having like primary palliative care where people are addressing those needs, or is it early palliative care in COPD where you’re getting early specialist level palliative care for these individuals with COPD?
Anand: Right. Great question. I have, as one of my mentors who sort of helped to bring about this field of early palliative care in oncology. And that’s at the time of diagnosis in Canon advanced cancer. So that’s a little bit trickier. It’s hard to say, you can do early palliative care, in the diagnosis of COPD. But you would want a pulmonologist or a primary care clinician to have a basic set of primary palliative care and geriatric skillset, to start the process of whenever they see a patient, whether that’s at moderate severe COPD, or even more other stages, to recognize that they need to start initiating something. And then when things get a little bit tougher, refer over.
Anand: There are plenty of figures from CAPSI and other organizations that illustrate this nicely. The amount of the dose of Jerry Pal gets to be more and more as that person gets closer and closer to the end of life.
Eric: And in the study, and in talking with patients and family members, was there anything that surprised you as far as their needs?
Anand: Well, I think the coping one was just brought up so much. They didn’t have an idea of what to do with their illness. Like how to do things. One guy just talked about, it took him all morning just to bring up the energy and the will to go and empty his dog water bowl for his dog. And so he talked about that was his primary focus for the day, which was to get over there, change his water bowl for his dog. And I thought, okay, well that’s incredible. That’s lot of social isolation. There’s a lot of depression there, there’s a lot of physical mobility issues, how can we get a strength up? And I started thinking about all these things that I could do for an intervention, that could help him just do that, and that could make so much better quality of life for him.
Anand: But everybody sort of echoed this. And then, what we never do as pulmonologists is reach out to the caregivers probably ever, and they were bringing up all the same things for themselves. Once COPD was diagnosed in my loved one, their mood changed. They started getting angry. I didn’t know what to do with them. I was scared. I never left the house. I became socially isolated myself and fearful and anxious. I wish I could give them a can of air somebody said. So, they were starting to express a lot of anxiety. And, I’d seen it, but they were telling it to me and I had exemplary quotes in the paper, which were just fascinating.
Alex: You mentioned anxiety here, and one of the key themes that you describe are emotional issues. When I think about the patients I’ve seen with COPD, anxiety does seem to come to the fore more so than depression. And I wonder if that’s part of the physical manifestations of the illness itself. Being short of breath is a state that causes anxiety in many people. I wonder if that was born out in your research.
Anand: Yeah, that’s for sure. I mean, it’s like drawing back to Maslow’s hierarchy. You got to try to think about survival. And you’re going to think about, you’re going to be very anxious when you can’t breathe. So yeah, there’s a vicious cycle there that perpetuates itself. And I think that there’s often even a phenotype because these people have smoked their whole life. And so smoking, anxiety, depression are all intricately tied together, and self medicated by smoking. And so, depression exist in COPD and so I wouldn’t forget about that also.
Eric: All right, so we have these palliative care needs, these needs for early palliative care in these individuals. So just kind of restate them, coping with COPD, emotional symptoms, respiratory symptoms, illness understanding and prognostic awareness. What did you do next in your kind of research on this topic?
Anand: So simultaneously, I was also interviewing clinicians from palliative care and pulmonary medicine to get their take on early palliative care, and that was pretty eye opening. If you’re going to try to design any system level intervention or interventions at all, you need to be able to understand what the frontline clinicians are thinking about the field. And that was pretty interesting because we did a qualitative study where we interviewed pulmonary critical care clinicians and palliative care clinicians about early palliative care and COPD and found a lot of barriers and facilitators to bringing early palliative care to this patient population. They were in themes of like educational themes, clinical themes and operational theme. Those are the three big categories.
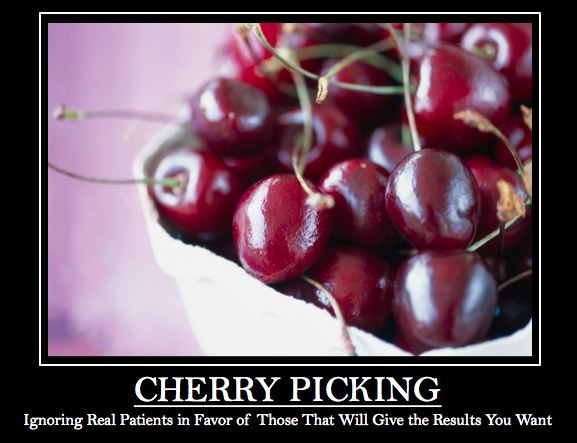
Anand: But fundamentally, pulmonologists were, like they do in cancer and like people do in oncology didn’t get the term palliative care correct.
Eric: How so?
Anand: I mean it was fundamentally interchanged over and over through the interview. It was only useful for end of life and it was often switched with hospice back and forth.
Alex: So it was synonymous with hospice and end of life care.
Anand: You probably heard that jazz too much.
Alex: Yeah, that sounds familiar.
Anand: But it’s more fascinating because pulmonary critical care we deal, we work with palliative care clinicians all the time in the ICU. So I was expecting to have some semblance of, you know what this is guys, but the critical care clinicians are trained to bring people back from the brink of death. It’s part of our score. We’re trained to intubate, to shock, to resuscitate. So that’s when I started to have that PalliPulm concept to somebody that can look at that person and think she’s 88, 92 years old with pneumonia, respiratory failure.
Anand: I can intubate. I can use high flow nasal cannula. I can think about opioid or morphine for Disney. I can start thinking about other measures in a fan event. And should I do it? Should I do this? What would be best interest for her? That kind of thing is the power of having both in your hands, pretty cool.
Eric: Do the pulmonologist have any other concerns about palliative care?
Anand: Yeah, so then they raise the clinical stuff, like when do we refer to palliative care? Aren’t they going to narc up my patients? Aren’t they going to give them too many benzos until they have a respiratory arrest? And then how are you supposed to add palliative care stuff to our already busy clinical life and is palliative care are going to be able to handle COPD? Because the numbers are infinitely larger than cancer.
Alex: Yes, huge numbers.
Eric: Do the palliative care doctors have similar concerns or what were their concerns, if any?
Anand: Yeah, so their concerns were close. I mean they recognized the misconceptions that pulmonologist would see, so they knew that those existed. They too were concerned about how to manage opioids and benzos and COPD, and when would be the appropriate triggers and how to prognosticate and COPD, and then would they have the bandwidth. So it paralleled nicely between both disciplines.
Alex: Do you want to say more about this concern about use of opioids and benzodiazepines in patients with preexisting lung disease?
Anand: I think it always refers to things like high chronic hypercapnia and that sort of hypoventilation state. You give too much opioids to somebody in that state, you may actually cause enough respiratory suppression to precipitate a respiratory arrest, and COPD that could lead to hypercapnia and acute hypercapnic failure. And where CHC might become somnolent, obtunded and need to be intubated.
Alex: Can you just say what hypercapnia is for our listeners who are not.
Anand: Great point. High carbon dioxide levels, and that’s what makes people sleepy, and people with COPD have high CO2 a lot, and makes them real tired and then they can become obtunded, which point I come in intubate. It happens all the time up here. It’s in the ICU. That’s one of the reasons for transfer.
Alex: Wait, sorry, is one of the reasons for transfer hypercapnia or is it opioid related hypercapnia?
Anand: I mean it can be opiod related hypercapnia or just hypercapnia from the COPD exacerbation.
Alex: So you believe that this concern about opioids leading to hypercapnia for patients with COPD, in other words, the opioid themselves slows down the respiratory rate so that people with COPD who are at risk for building up CO2 in their bloodstream already, that’s further exacerbated by the low respiratory rate and they’re not blowing off that CO2, that CO2 accumulates in their bloodstream, makes them sleepy, they are unable to protect their airway, and they’re at risk for not breathing.
Anand: Right. That’s exactly right. I mean, I’m not stating it as I’m opposed to it, rather, I think it needs to be a combined effort between a palliative care clinician and the pulmonologist working together to find the right dose that would be safe enough. And I have had patients personally who have started low dose opioids and have had tremendous benefit in relieving their dyspnea. So it’s not without question that it could help, it’s just something that’s a lot different clinically than someone with cancer where you could do that a little bit more freely.
Eric: And I also want to refer to our listeners if you want to learn more about dyspnea, both in COPD and cancer. We did a podcast about a month ago with David Caroll from Australia, really great topic. We talk a lot about the research behind this, including the evidence base for opioids and dyspnea. And I think one of the key take homes is usually those are smaller doses of opioids given as long acting medications. But again, I really encourage you to listen to the David Caroll Podcast.
Alex: Interested to hear what you use when you say, low dose opioids, what are you using?
Anand: Like oxycodone, like five milligrams twice a day as needed, something like that. And I would find that won’t hurt anybody.
Alex: Twice a day. The half life is short enough that it’s like four to six hours or something, but you give it twice a day.
Anand: Yeah, I’d probably be okay with that.
Alex: Yeah. But in more than that, you might be concerned.
Anand: I’d be a little bit more concerned. But again, I’m still just starting out, so…
Alex: Right, right. Would you ever use liquid morphine?
Anand: Yeah, in the inpatient setting I would use two milligrams IV morphine, but I can see them in visual and watch them and I’d get a much more frequently and I’ve observed that and I can see it and I’m okay with that.
Eric: And just a shout out to our listeners. Again, I think for me, the one big take home from David Currow was like all these are long acting opioids, but they have formulations of long acting that we don’t have here in the U.S. generally, which is lower dose. So someone out there give us a low dose long acting format.
Alex: We need that. And the other take home from the David Currow podcast was, for people with moderate to severe shortness of breath who were started on a long acting opioids, there were no harms in terms of a respiratory depression that rose to the level of clinical alarm.
Eric: Yeah. In the studies using low dose long acting opioids.
Anand: Right.
Eric: So how does that convert to clinical medicine is another question.
Alex: Right.
Anand: Yeah. And I mean, and some studies have shown some adverse events in older adults in particular, so we do have to be cautious about the opioids and benzos in that population anyway. So just keep throwing it out there.
Eric: So going back to kind of what you’ve learned from the palliative care doctors, the pulmonologists, was there a consensus of who should get kind of specialty level palliative care?
Anand: Yeah, probably. I mean people gave some referral criteria and almost all of them thought the clinician side thought you get a certain FEV one in the 50%, so that would put you at around moderate or severe to very severe COPD for using these stage and criterias. So long function on a pulmonary function test, people who have severe shortness of breath, frequent hospitalizations became brought up as criteria. If you’re admitted in you or you get mended to the ICU in particular. I don’t know if you guys know that, but a person who’s admitted for a COPD exacerbation, one in four may die in the year after that. And one and two will die within four years.
Anand: So, a severe exacerbation is a pretty sentinel event for COPD. So everything that you saw in residency and admitted, those people have a high mortality in the next year. So that’s an immediate trigger for me that they probably need some palliative care at that point. Starting things like bypass and or having things like depression and anxiety. But the list was huge, what could be brought up with frequent hospitalizations kept coming up over and over.
Eric: Yeah. So it sounds like part of that is from a prognosis stand point, their prognosis may be significantly worse. So I think about COPD too. I think one of the challenges is prognostication. Like I can look at like the boat index, is a boater Bodhi.
Anand: Yeah, I thinks both. Yeah, I do both.
Eric: All right. The boat index, which doesn’t really help you is it gives you like a four year prognostic idea based on courthouse. I don’t find it incredibly helpful. How do you think about prognosis and COPD?
Anand: Good question. I mean, I think of it, you’ve seen everybody that has, I’ve seen people with the worst lung function you can imagine live for years. And so that’s the challenge with we would treat face and putting palliative care to a chronic disease state is this longer lifetime that they have it with way poorer quality of life in many senses than some with advanced cancer.
Anand: And Emmy Kelly put out a great paper that said that they, people with COPD, dyspnea, nausea, vomiting, pain, anxiety, all of this off and on in proportion with advanced cancer. How do you prognosticate? I mean I think it’s an individual level, without using the scores. We know what the scores can do, but you still kind of say, you still try to paint that picture of the unknown trajectory, and bringing, raise that up to the patient and just being honest with them about, we don’t know that trajectory, but we do know some data, we have some data we can tell you, but you could live a long time, but here’s what we do know.
Anand: Your lung function will decline over your lifespan. You won’t be able to walk to the mailbox and back next year. You may not be able to. In two years you might not be able to get out of your house. And so I started talking, I started painting realistic things. I start drawing in their life space for them and start using that to guide me with their prognosis. So like, What do you want to do? Oh, I just want to get up and down my steps of my apartment. Oh, okay. We can do that. You want to go walk to your church, which is a mile away. I don’t see that happening right yet unless we do a few things. So I tied into simple stuff.
Alex: Yeah, that was a great segment. Just there you just highlighted three incredibly important concepts and probably more. One, acknowledging and normalizing the uncertainty, inherent prognosis for patients with COPD, so much less predictable in terms of mortality than cancer. But nonetheless, there is predictably going to be a loss of function and that you framed that in terms of what people care about, particularly older adults. How are they going to get around and get out to do the things they enjoy doing, and how is that going to change over time? And that you framed that in terms of the concept of life space. Which is a contribution from UAB, University of Alabama at Birmingham.
Anand: Yeah, shout out to Richard Allman and Cynthia Brown and Patricia Sawyer or some of the creators of that instrument.
Alex: Anand, could you just say a little bit more. Few of our listeners are researchers, but many of them will intuitively grasp this concept of life space. I want to just give you an opportunity to get on a soap box. Talk about it a little bit.
Anand: Yeah, sure. I’ve been setting live space and COPD in parallel to this because I think it’s just a fascinating concept. Cynthia Brown, Richard Allman were some of my mentors about 15 years ago here at UAB as a young whipper snapper undergrad studying sort of geriatrics principles here. And my space is sort of your immediate surroundings, it’s the… But it’s an instrument that was developed here that calculates your distance, your frequency and independence of movement among five live space levels to your rooms and where you sleep, around your house, immediately outside of your house to your neighborhood, and outside your town. And it paints this beautiful picture of how somebody can go from one room all the way outside of their town, and attracts nicely with numerous outcomes in older adults, and the UAB’s study of aging. It predicted nursing home admissions, hospitalizations, mortality.
Anand: So when you say you’re restricted in your life space, there’s a certain score that will predict with reasonable certainty, you can get admitted to a nursing home pretty soon if you’re an older adult. And I found that restricted life space in pilot study, predicts the COPD exacerbation and tracks nicely with many functional outcomes for COPD patients.
Alex: And what I like about what you did just there a moment ago was to describe how a person’s life space would be impacted by disease progression. In other words, as their disease progresses, their life space is likely going to constrict. And yet you were finding out what’s important to them and aligning those important activities with ways that you might be able to accommodate, help support them to improve their quality of life, which is terrific.
Anand: Yeah, we need payer support though, because you imagine something as simple as supplemental oxygen. And you think about a frail, tiny older female with COPD which weighs 95 pounds, asking her to tote a five to 10 pound oxygen tank around. That becomes a tether, right? You guys love the term. I put my geriatrician hat, I’ve got to figure out a way to get that tether, not to keep her in the house. Because she wants to wear her diamond earrings and go to church, and she doesn’t want to be kept and use that tethered to keep her at home. And I get that all the time. That’s a weekly occurrence. This is going to trap me in my home. This is a ball and chain. How am I supposed to tilt this thing around?
Anand: But if you think about it, they often don’t leave their room because of their supplemental oxygen. It’s a fall hazard. The tubing goes around the house or about the trip all over it, and they can’t get, it’s both liberating and trapping at the same time. And so I think of it at an end of geriatricians mindset. Oh my God, I got to figure out making sure they don’t get stuck at home because of this thing. It’s just a simple way.
Eric: And you, you brought up payers and potentially system’s fact. Because I’d love to talk just briefly about the American journal of medicine article that you published also on end of life spending in healthcare utilization for these COPD patients, older COPD patients. Is it okay to kind of summarize kind of what you did then in that argument, and what you found?
Anand: Yeah, that was a retrospective study of Dartmouth Atlas data and older decedents with COPD, we had 140,000 decedents with COPD older than 65 years. We examined spending and utilization in the last two years of life. So these are decedents who died in 2013 to 2014. We looked at overall spending and categorical spending across inpatient and outpatient categories. 40% of the spending came from inpatient, but the remaining 60% went to all sorts of other ambulatory services.
Anand: Utilization was through the roof. As you can imagine, roughly 80% were admitted to the hospital in their last years of life, half were admitted to an ICU. The length of stay was very high. But what was amazing to me was that, as a population health standpoint, there was tremendous variability across the country, in ways that different peripheral regions spent and utilized. I guess it’s like if you build it, they will come mentality, highly populated urban centers had high rates of utilization and longer lengths of stay and those things track nicely.
Anand: But the takeover was more so than that was the hospice utilization. We hadn’t had any real concrete data on hospice in COPD. I went into this knowing that palliative care was very abysmally utilized when we’re talking 1%. Any study that I read was like 1% of this sample, 1% of that sample. It was a tremendous increase from 0.3 to a 0.9%, something like that. That’s what I’ve read over and over and over. Well, that’s just sad. And I knew that the data from things like an HPCO or Hospice and Palliative Care Organization, was that roughly 50% of older decedents get hospice, the end of life.
Anand: And we found something similar about 47% of older COPD decedents received hospice. And though currently from what I can tell, the average length of say an office is 70 days for the average population, and that’s been kind of growing solely over the last few years. In that time period, ours was 39 days on average. So COPD patients are going real late, and hospice didn’t track with spending like all the other categories did.
Eric: What do you mean by it didn’t track with spending?
Anand: It meant that all the other category things like acute care, length of stay, elTec length of stay, and skilled nursing facilities, all of those had some association. You had more utilization of it, the spending increased. But with hospice, things were pretty flat across the… There was a linear association with spending there. And so, my take home was that we were referring too late. There was widely variable geographic utilization. Some places were super low, some places were decently high. But if we’re going to try to make an impact on outcomes like has been shown in cancer, they can’t wait until the last month alive to do this. So that’s why you need early palliative care.
Eric: So what’s next for you? So you’ve taught us that there’s high symptom needs, emotional needs, coping needs for individuals with COPD, huge utilization issues, healthcare utilization that we’re not using palliative care early enough. What’s next for you?
Anand: Yeah, that’s a great question. So there’s a lot of unknowns in the next few months, but all this data provided a tremendous background data for a grant that’s out there. And so, depending on how that goes, that’s what I’m trying to build an intervention, an early palliative care intervention model by prior successful early palliative care interventions in cancer tailored to older adults with COPD specifically focusing on things like life space and physical function, frailty, those kinds of things, and see how this kind of intervention can impact it using a pilot trial mechanism. So that’s what I’d like to do. Make the career bigger. Get the pulmonologists, knock them on the head, tell them we need to do these things more.
Alex: That’s great. Yeah. Teach them what palliative care is. PalliPulm.
Anand: That’s exactly right, yes.
Alex: It’s not hospice. Hey, have you heard of other programs that have a PalliPulm? Are there successful models elsewhere in the country of outpatient palliative care clinics for example, that are seeing quite a few patients with COPD?
Anand: There was one in Canada where they integrated for interstitial lung disease pretty well. They integrated palliative care using nurse practitioners. I’ve had some colleagues in Illinois and elsewhere embed a palliative care clinician in their pulmonary clinics. Those are reasonable and seem to be our scalable options. But I think it’s going to have to be that, you guys know this, there’s not enough to go around and we need pulmonologists and primary care clinicians to get the message and learn the skill sets if we’re going to have a chance to meet the deficit of palliative care and geriatricians that’s coming in the next decade.
Alex: Yeah, absolutely. We need models like enable, which is right. Telephone-Based Nurse-Led, isn’t it? In intervention. We’re going to have a podcast with Marie Makitas in a month or so.
Eric: Yeah, I’m excited about that.
Eric: Yeah. Learn more about enable.
Anand: Yeah, that’s what my interventions modeled after, and I know it’s sort of preliminarily feasible and patients with COPD now we just need to tailor it to the older adult population. But we just need to make sure that pulmonologists know what palliative care is. That’s a pretty problem.
Eric: Well there’s things I think that pulmonologists need to know. I’m wondering, are there a couple of things that as geriatricians or as palliative care clinicians that you really wish that we knew or pet peeves that you have?
Anand: Yeah. This is a tough question. I don’t think you guys see enough of them to maybe get the experience that I, even in my study care clinicians were concerned about what medicines, like antidepressants and anxiolytics would do to COPD patients. And I think if you gave us a call, we could work together to find a right dose that would be safe. And we’ve did this discussion throughout this podcast, right, that opioids are not necessarily harmful, but if you do it at the right dose, we might be able to work together. Then talking with us about prognostication, I’m one that can bring it up early, but some of my colleagues don’t want to refer to you guys because they feel like people are throwing in the towel, and I don’t think that’s right. I think that you’re going to have to work with us and figure out what that prognosis means and how do you define that better.
Eric: I got another question for you. So I’m really excited about PalliPulm. I want to learn more about it. Actually we are here at our institution, we’re actually working on trying to get palliative care integrated with pulmonary chest clinic with Neal Trivedi and others like that. If I want to kind of dive deeper into this, what can I do to get more involved in the PalliPulm community?
Anand: Well, we’re on Twitter. That’s where we started at PalliPulm, and you can pull up all the hashtags, using the model of this famous podcast that I’ve heard about called Geripal blog…
Eric: I heard about that before.
Anand: Yeah. We’re trying to do this similar model and build that this year. That’s the goal for this year is to start… Because I thought, I know people across the country and over across the world that are interested in this topic. They have to exist, and in the course of nine months I found 1200 people.
Eric: Wow.
Anand: So this is worldwide. We have people all over India that are tagging hashtag PalliPulm that are like, wait a minute, this is what I do. I’m an interventional pulmonologist. I love this concept. And so then you’ve got people… Currently, one of my mentees, Dina Khateeb, who is at Mount Sinai finished her pulmonary critical care fellowship now doing a year in palliative care up there in Mount Sinai.
Anand: So, you’ve got people that exist in the world where we’re putting a face and a title to it, and then soon we’re going to provide a resource where people can come to find out more information, probably online. And it would be a blog format.
Eric: What about a podcast?
Anand: Sounds like a great idea. So that’s something we need to start thinking about how to do and doing it.
Alex: Do you play the guitar?
Anand: I play piano.
Alex: Piano, then it’s got to be different. Love it.
Eric: Well, I learned a ton. I want to thank you for joining us. Anything else you want to talk about with PalliPulm.
Alex: No, man, this is it. I love it. I appreciate it guys. Thanks for giving me a place to talk about it.
Eric: Well, you can’t leave now because we got a little bit more song left. Let’s hear it, Alex.
Alex: (singing)
Eric: I can always tell when Alex loves playing a song.
Eric: Well, again, a big, big thank you for joining us and to all of our listeners for joining us and supporting the Geripal podcast. If you would like to support the Geripal podcasts, you can always go to your favorite podcasting app and rate us. And now, Alex, what’d you say?
Alex: I said thank you to Archstone foundation.
Eric: Goodnight everybody.
Alex: Bye folks.