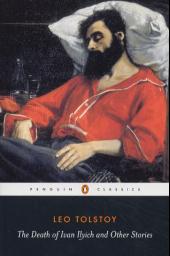
This week’s Lancet includes an article titled “The Death of Ivan Ilyich and pain relief at the end of life” authored by Guy Micco and GeriPal’s very own Alex Smith and Patrice Villars (it can be viewed for free if you register). This is a thought provoking article focused on the question of whether there is overuse of pharmaceuticals to treat various forms of suffering in hospice and palliative medicine. It also serves as a nice follow-up to Patrice’s post on the geriatric care of the hospice patient.
The authors argue that a good death, as seen through their interpretation of The Death of Ivan Ilyich, may include physical and existential suffering. Tolstoy’s character finds redemption in his suffering; he remains conscious through the agony of a prolonged and painful death and ends up with a greater understanding of life. The authors further argue that such a moment of clarity may no longer occur if we rely on practices that promote complete freedom from suffering through the over use of pharmaceuticals:
“What would happen if Ivan Ilyich—a modern day “John Doe” or “Everyman”—were dying in the USA now? At home or in the hospital, it could be the same story: when he became unable to speak coherently for himself, his wife or perhaps the ward or hospice nurse, seeing him flail and hearing him scream, would request morphine and ever-more morphine. And, if that did not work, something would be found that would work to extinguish the visible signs of discomfort: lorazepam, haloperidol, phenobarbital. Drugged, but without “pain”, what would become of Ivan Ilyich’s inner experience? Would it be transformed? Would it go away?”
My immediate thoughts after reading this paragraph turned to the increasing use of symptom scores to assess quality in hospice and palliative medicine (just this week I finished reading one bereavement survey where the benchmark was NEVER having pain). By setting a one-size-fits-all benchmark of quality on complete pain relief we may be going against the very foundation of palliative care – respecting patients’ and families’ values and preferences regarding end-of-life care. Some patients may value lucidity over freedom from physical discomfort; recognizing this would be a true measure of quality in hospice and palliative care.
What do you think? Do we, as a hospice and palliative care community, have an over reliance on the pharmaceutical relief of suffering, whether it be from pain, anxiety, or “agitation”? Is Tolstoy’s idea of a good death “redemptive” for some leading to “self-understanding or spiritual awakening”? Did the authors misread Tolstoy (was his death even redemptive?)



